|
ALD 2021 VIRTUAL CONFERENCE
APRIL 8-10, 2021
Dentistry’s Laser Meeting | 24+ CEUs | Stay at Home | Live & On-Demand Access
ABSTRACTS
Listed by Date and Time
| THURSDAY, APRIL 8, 2021 |
 |
9:15 AM - 10:00 AM
Samuel Low, DDS, MS, MEd | Palm Coast, Florida, USA
The New Standard of Care in Managing Peri-Implant Disease
Track: Implantology
Audience: All
While inflammation associated with dental implants is at an all-time high, we can prevent loss of implants with innovative chairside techniques to reverse implant mucositis and also show success via minimally invasive techniques with bone loss implantitis. Long-term implant survival can depend on quality prevention, treatment and maintenance. The dental team (especially the dental hygienist) can have successful systems and tools to enhance longevity and implant health. A recent landmark study demonstrates validity in managing peri- implant disease with all-tissue-erbium lasers. Clinical research shows how erbium laser wavelengths have been incorporated into procedures for treating peri implant disease with no adverse thermal events as to the integrity of implant surfaces. Dentistry is evolving into a minimally invasive culture with attention to positive patient perceptions and comfort We will define user friendly protocols, establishing systems related to severity of implantitis with expectations. Patient talk tracks for positive case acceptance will be reviewed.
Educational Objectives
- Explore the etiology of implants disease from both a microbial and surface corrosion perspective
- Develop an understanding of the erbium wavelength as related to the effects on target tissue for implants
- Describe the effect of erbium lasers on various titanium surfaces as part of a detoxification process in managing peri implantitis
Laser Information: 2780-nm Er,Cr:YSGG laser (Biolase, Foothill Ranch, Calif., USA), 1.5 Watts, various tip diameters and configurations
|
| |
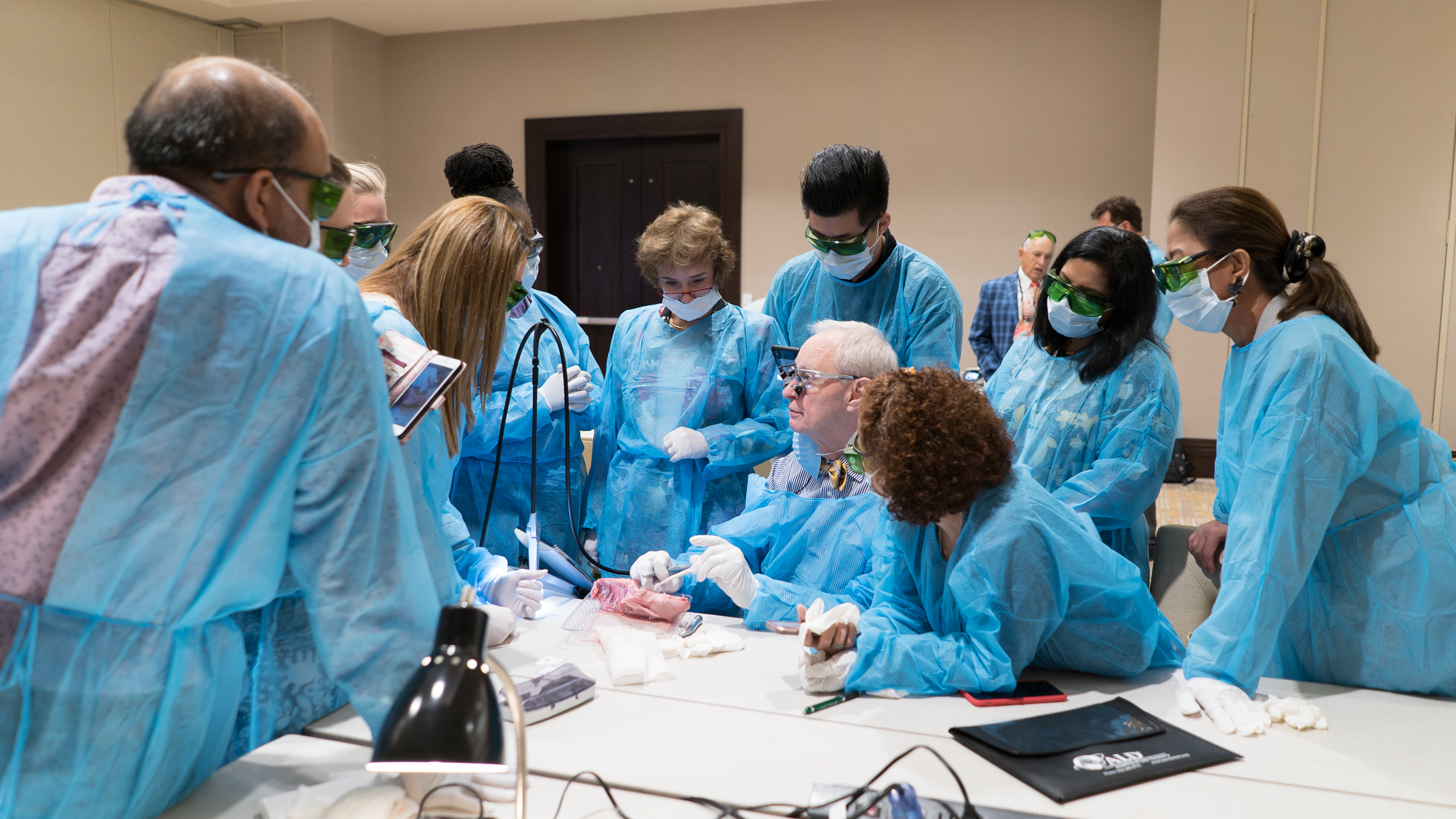
10:00 AM - 11:00 AM
Samuel Low, DDS, MS, MEd | Palm Coast, Florida, USA
A “How to” Live Demonstration for the 5 Most Frequent Laser Uses
Track: Demonstration Course – Laser Applications
Audience: All
Create value-added revenue with a step-by-step interactive instruction of laser applications in the practice of all phases of dentistry. Experience positive results with diode and erbium laser wavelengths from soft tissue to periodontal applications. We present procedures including nonsurgical laser bacterial reduction, laser-assisted periodontal therapy (LBR, LAPT)/surgical periodontics, frenectomy, gingivectomy, biopsy/fibroma, and crown lengthening. With the technology of visualizers, you will observe real-time demonstrations with your input for interaction. You gain insight into each procedure in a step-by-step fashion to instill confidence when you return to the practice.
Educational Objectives
- Review pocket access and pearls for LBR, LAPT, and microsurgical flap exposure for periodontitis and peri-implantitis treatment.
- Understand indications for using lasers in crown lengthening and pre/post-orthodontic procedures including esthetics.
- Learn procedures for the most common soft tissue issues in restorative dentistry.
- Develop postoperative evaluation protocols assessing wound healing.
Laser Information: 940-nm Epic X diode laser, 980-nm Epic Hygiene diode laser, 2780-nm Er,Cr:YSGG laser (Biolase, Foothill Ranch, Calif., USA). Parameters will vary depending on the procedure.
|
 |
10:15 AM - 11:00 AM
Robert Miller, MA, DDS, FACD | Jefferson, Oregon, USA
Treatment of Peri-Implantitis Using UVC Lasers
Track: Covid-19
Audience: Novice
Dental professionals are routinely exposed to aerosols generated by a variety of dental instruments. These aerosols contain potential pathogens and represent serious health risks to the professional. The high-speed turbine handpiece is the most obvious aerosol generator, but other instruments like sonic and ultrasonic scalers, hard tissue lasers, and even the air-water syringe also contribute significant aerosols. To address the risks from these aerosols, dentistry has adapted universal precautions for infection control and personal protective equipment (PPE) recommendations. In light of the COVID-19 pandemic, current PPE recommendations include an appropriate rated respirator or mask for the procedure, face shield, head cap, gown, gloves, and shoe coverings to reduce the exposure and potential spread of infectious diseases. These help to protect the professional from exposure, but do nothing to minimize the potential pathogenicity or control of the origin of the aerosol during the procedures. This program will present strategies to reduce the health risk of the dental aerosol with preprocedural rinses and also to control the aerosol with extraoral vacuums.
Educational Objectives
- Discuss the health risks of dental aerosols for dental professionals.
- Examine recommended measures and additional strategies to reduce disease transmission from dental aerosols.
- Implement simple universal dental aerosol strategies.
Product Information: 99.99% high-efficiency particulate (HEPA) extraoral vacuum (DAX, Dental Safety First, Albany, Ore., USA); Carifree preprocedural rinse (0.20% sodium hypochlorite) (Oral BioTech, Albany, Ore., USA)
|
 |
11:00 AM - 11:45 AM
Robin D. Horton, BDS | Harpenden, Hertfordshire, United Kingdom
How Digital Technology Enables Safer and More Accurate Implant Planning and Computer-Guided Surgery
Track: Implantology
Audience: All
This presentation will start with cone beam computed tomography (CBCT) and intraoral scanning (IOS), describing their strengths and weaknesses and what to look out for. Included are some general safety data and rationale for always using CBCT when planning implant surgery. Discussion includes how to collect the data and import into implant planning software (DTX Studio Implant, Nobel Biocare, Kloten, Switzerland) or directly into the new X-Guide (X-Nav Technologies, Lansdale, Pa., USA) surgery machine itself. This enables the clinician to rapidly plan, make virtual setups, and create a virtual surgical guide in minutes. A visual guide machine can then be used to place the implant accurately using video cameras to pick up markers, one fixed on the patient and one fixed on the surgical handpiece, to give turn-by-turn directions. The clinician can more confidently place implants, providing an achievable margin around vital structures, and lining up implants easily with each other. With the new advances in X-Guide and the X-Mark (X-Nav Technologies) probe tool, one can change the plan as one goes along if needed. There is no more waiting for a printed guide to come back. Access is easier as normal-length drills are used with the visual-guided machine.
Educational Objectives
- Explain why CBCT is crucial in safe implant dentistry.
- Understand how to bring data together from different sources to enable visualization of the final proposed result to ensure predictable and excellent planning.
- Appreciate why guided surgery is safer when placing implants than freehand, and which systems are the most accurate.
- Learn how to take a digital scan of the emergence profile.
Laser Information: 2780-nm Er,Cr:YSGG laser (iPlus, Biolase, Foothill Ranch, Calif., USA) for opening site and socket debridement. 940-nm diode laser (Epic X, Biolase) with healing wand for photobiomodulation
*Sponsored by Nobel Biocare UK
|
 |
11:30 AM - 12:15 PM
Akira Aoki, DDS, PhD | Tokyo, Japan
Er:YAG Laser-Assisted Comprehensive Periodontal Pocket Therapy (Er-LCPT)
Track: Implantology - Laser Research Periodontology
Audience: All
Lasers are increasingly being used in periodontal therapy because of various advantageous therapeutic effects such as ablation, hemostasis, bactericidal effect , and biostimulation. The Er:YAG laser is among the most suitable for periodontal treatment because it exhibits effective ablation of periodontal hard and soft tissues, with minimal thermal side effects, and thereby does not impair wound healing. Root and bone surfaces can be treated with this laser. In particular, enhancement of bone regeneration following Er:YAG laser debridement has been suggested in an animal study. To date, numerous clinical studies for periodontal pocket treatment using an Er:YAG laser have been published and some have reported positive results; however, a consensus has not yet been reached regarding its effects due to differences in methods and parameters of irradiation for pocket therapy. This presentation reviews the basic and photobiomodulation (PBM) effects of an Er:YAG laser on periodontal tissues as well as the findings of previous clinical studies for pocket treatment. Then, a novel procedure using an Er:YAG laser combined with conventional mechanical treatment (Er:YAG laser-assisted comprehensive periodontal pocket therapy: Er-LCPT), is introduced. Er-LCPT is a minimally invasive flapless surgery that enables safe, effective, and comprehensive debridement of periodontal pockets. In the treatment of residual pockets, the effectiveness and safety of this procedure have been confirmed by case series. Also, significantly improved outcomes of clinical parameters have been detected by a randomized controlled trial of Er-LCPT when compared to scaling and root planing (SRP) alone. Er-LCPT may also be used as a regenerative therapy in limited cases.
Educational Objectives
- Enumerate the advantageous characteristics of the Er:YAG laser in periodontal therapy.
- Explain the current clinical status of the Er:YAG laser in pocket treatment.
- Understand the concept, procedure, and effects of Er-LCPT technique.
Laser Information: Er:YAG laser (Irwin AdvErl EVO, J. Morita, Kyoto, Japan)
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
12:15 PM - 1:15 PM
Moderator - Walid Altayeb, DDS, MScD, PhD | Abu Dhabi, United Arab Emirates (UAE)
Panelists - Akira Aoki, DDS, PhD; DDS; Robin D. Horton, BDS; Samuel Low, DDS, MS, MEd; Robert Miller, MA, DDS, FACD
A Panel Discussion: Lasers in the Treatment of Peri‐Implant Disease: Benefits, Limitations, and Potential Risks
Tracks: Implantology, Periodontology
Audience: All
Peri‐implant diseases are a growing concern in recent years and stand as a great challenge for clinicians, especially since there is no standard of care for peri-implant diseases and clinicians are faced with many choices when deciding upon a method of treatment. Appropriate laser‐assisted peri-implantitis therapy may provide additional benefits compared to traditional treatment. Nevertheless, it is difficult to draw specific conclusions about the clinical outcomes. This difficulty is due to several factors, including a wide diversity in the types of lasers, energy settings, and modes of delivery utilized, in addition to the heterogeneity and potential for bias among studies.
The panelists will discuss the possible benefits, limitations, and potential risks of laser therapy of peri-implantitis based on clinical expertise and best evidence.
Educational Objectives:
- Address the possible benefits of using lasers in the treatment of peri-implantitis.
- Identify the limitations of some laser wavelengths in peri-implantitis treatment.
- Highlight the potential risks of different laser wavelengths to dental implants and surrounding tissues.
- Specify possible safe and efficient laser wavelengths and protocols for the treatment of peri-implantitis.
|
|


|
3:00 PM - 4:00 PM
Sebastiano Andreana, DDS, MS | | Buffalo, New York, USA
Sam Low, DDS, MS, MEd | Palm Coast, Florida, USA
Edward R. Kusek, DDS, Sioux Falls | South Dakota, USA
Diode Lasers for Therapy of Peri-Implantitis
Track: Controversies in Dentistry
Audience: All
The presentation will focus on the clinical applications of 810-980 nm diode laser wavelengths for therapy of peri-implantitis. Diode lasers are used with dual purposes, for their antimicrobial effects and their biostimulating effects. This lecture will show the techniques with clinical cases, focusing on the safety of the procedures, and supporting the procedures with findings from laboratory studies.
Educational Objectives
- Summarize the clinical applications of diode lasers for treatment of peri-implantitis.
- Describe the safety of using diode lasers for treatment of peri-implantitis.
- Identify the clinical techniques of using diode lasers for treatment of peri-implantitis.
Laser Information: 810-nm Odyssey Diode Laser (Ivoclar Vivadent, Amherst, N.Y., USA), range 0.2-0.8 Watts in continuous mode, in contact and non contact; 810-nm Photon Diode Laser, (Zolar Technology, Mississauga, Ontario, Canada), range 0.2-0.8 Watts in continuous mode; 970-nm Sirona SIROLaser (Dentsply Sirona, Bensheim, Germany)
|
 |
4:00 PM - 4:45 PM
Keith Brewster, DDS | Dallas, Texas, USA
Overview of CBCT, CT, MRI, and PET Scan Technologies
Track: Esthetic Dentistry - Digital Dentistry
Audience: All
This presentation compares computed tomography (CT), magnetic resonance imaging (MRI), and positron emission tomography (PET) scans of the same anatomical areas and shows what information can be learned from each scanning modality.
Educational Objectives
- Define different scanning technologies.
- Specify the objective information-gathering capability of each scan modality.
- Appreciate the information gathered and each discipline’s strengths and limitations.
|
 |
4:45 PM - 5:30 PM
Kenneth Luk, BDS, DGDP (UK), MGD (CDSHK), MSc (Hong Kong) | Hong Kong Special Administrative Region (SAR), China
Use of a 445-nm Blue Laser in Clinical Dentistry
Track: Esthetic Dentistry
Audience: All
The blue diode laser wavelength (445 nm) has been available to the dental market for 5 years. It is a relatively new laser compared to near-infrared diode lasers. The optical properties and tissue interaction of this wavelength offer additional benefits in clinical applications. This case series demonstrates the use of the 445-nm diode wavelength as a soft tissue surgical laser and its application in photobiomodulation. Whether the blue wavelength will replace other diode wavelengths will also be discussed.
Educational Objectives
- Discover the optical properties of the 445-nm laser wavelength.
- Describe laser-tissue interaction of this wavelength.
- Enumerate clinical applications of the 445-nm laser wavelength.
- Specify advantages and disadvantages of this wavelength.
Laser Information: 445-nm diode laser (SiroLaser Blue, Dentsply Sirona, Bensheim, Germany), CW output power 0.6 to 2 W, 320-µm fiber, 5 mm rod. Parameters vary for the demonstrated clinical procedures.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
5:30 PM - 6:00 PM
Hanaa Nassar, DDS, MSc, PhD | Cairo, Egypt
The Esthetic Blend Factors: Combining Ultraconservative Veneer Rehabilitation and Laser-Assisted Periodontal Therapy
Track: Esthetic Dentistry
Audience: All
When definitive esthetic rehabilitation is required, conservative treatment comprising morphologic modifications should be considered as a first therapeutic option. Ultraconservative additive rehabilitation strategies utilizing recent adhesive technology in combination with advanced ceramic materials and laser protocols allow practitioners to not only create highly esthetic and natural smiles, but also maintain the balance between pink and white esthetics and provide the patient with a faithful reproduction of natural teeth with notable morphological and color stability and excellent periodontal biocompatibility. No-prep and minimal preparation additive veneers are considered an excellent treatment option for certain esthetic challenge, and when both hard and soft tissues are properly manipulated, clinical longevity can be guaranteed. This lecture will discuss an ultraconservative additive esthetic rehabilitation protocol through the combination of minimal preparation veneers and laser-assisted periodontal treatment. Benefits as well as shortcomings of prep-veneers will be discussed.
This presentation will also highlight the guidelines for case selection with illustrations of different cases that require additive interventions. Moreover, full digital work flow for case planning and treatment execution as well as a systematic protocol for predictable bonding will be explained.
Educational Objectives
- Examine the guidelines and protocols suggested for case selection for minimal or no-prep veneers and verify the cases that require laser-assisted periodontal therapy.
- Recognize the laser-based protocol for soft and hard tissue treatment for optimum results and longevity.
- Discuss the protocols for minimally invasive veneering of discolored teeth and cases that require laser-assisted gingival depigmentation.
- Convey and implement the clinical protocol for preparation and bonding of veneers to ensure clinical success.
Product Information:
1. CAD/CAM Scanners: Identica Blue extraoral scanner (Medit, Seoul, South Korea); inEos X5 scanner (Dentsply Sirona, Charlotte, N.C., USA).
2. CAD/CAM software: Exocad DentalCAD (exocad, Darmstadt, Germany); CEREC 15.0.0 (Dentsuply Sirona, Charlotte, N.C., USA).
3. 5-axis milling machines: CAM 5-S1 Impression (vhf camfacture, Ammerbuch, Germany); CEREC inLab MC X5 (Dentsply Sirona, Charlotte, N.C., USA).
4. Digital shade guide: Vita Easyshade V spectrophotometer (VITA Zahnfabrik, Bad Säckingen, Germany).
5. Laser device: Waterlase Express (Biolase, Foothill Ranch, Calif., USA), 2780 nm, free-running pulsed, Average Power 0.1-4.0 W, Pulse Energy 0-250 mJ, Fiber/Tip Diameter 200-1200 µm.
|
 |
6:00 PM - 6:30 PM
Sara Kassem, MSc, PhD | Cairo, Egypt
An In Vitro Comparative Scanning Electron Microscope Analysis of Desensitizing Toothpaste and Diode Laser, Alone or Coupled, for Evaluation of Efficacy of Dentinal Tubule Occlusion
Track: General Dentistry
Audience: All
Objective: The objective of this study was to compare the dentinal tubule occlusion capabilities of nano-hydroxyapatite (nHAp)-containing desensitizing toothpaste and diode laser, alone or coupled.
Materials and Methods: Twenty-eight mid-coronal dentin discs were prepared from intact human premolars extracted for orthodontic purposes. The discs were immersed in 1% citric acid for 20 seconds to expose the dentinal tubules to simulate sensitive teeth and then randomly divided into four groups (n = 7). The control group (I) received no desensitizing treatment. The experimental group (II) was treated solely with a commercial nHAp-containing desensitizing toothpaste (Biorepair, Coswell, Funo di Argelato, Bologna, Italy). Group III was treated solely with a 980-nm diode laser (Simpler, Doctor Smile, Brendola (VI), Italy) in noncontact mode for 60 seconds. Group IV was treated with both toothpaste and diode laser. After toothpaste and laser application, specimens were subjected to acid challenge to analyze the resistance to tubule occlusion. After treatment, analysis of occluded dentinal tubules was done by scanning electron microscope (SEM).
Results: SEM analysis revealed that all the experimental groups noticeably occluded the dentinal tubules, and the extents were complete after application for 7 days. The majority of the occlusion was still preserved even after acid challenge. Group IV showed the most dentinal tubule occlusion in comparison to other groups.
Conclusion: Diode laser application has shown more efficacy than nHAp-containing toothpaste in dentinal tubules occlusion, while combining both methods resulted in a higher efficacy.
Educational Objectives
- Evaluate the effect of desensitizing toothpaste and diode laser on dentinal tubules.
- Characterize the histological changes in the dentinal tubule following laser irradiation.
Laser Information: A 980-nm diode laser (Simpler, Doctor Smile, Brendola (VI), Italy) was utilized for the procedure, operated at 1 W of power in noncontact mode for 60 seconds.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
6:10 PM - 6:20 PM
Yujin Ohsugi, DDS, PhD | Tokyo, Japan - Dr. Eugene Seidner Research Grant Recipient
Sayaka Katagiri, DDS, PhD | Tokyo, Japan
Novel Bone Regenerative Therapy: Sequential Microarray Analysis of Er:YAG Laser-Ablated Bone Tissue and the Modification of Gene Expression in Osteocytes and Osteoblasts
Track: Seidner Research Grants Scholar
Audience: All
Background: The Er:YAG laser has been applied for bone ablation during periodontal and implant surgery, anticipating advantageous effects other than just mechanical ablation. However, the effect of Er:YAG laser irradiation on bone healing remains unclear. The aim of this study was to evaluate comprehensive and sequential gene expression in laser-ablated bone, bur-drilled bone, and non-treated control bone to clarify the biological responses for bone healing.
Materials and Methods: Male Wistar rat (10-week-old) calvarial bone was ablated using an Er:YAG laser (wavelength 2.94 µm; DELight, HOYA, ConBio, Fremont, Calif., USA) or steel bur (10,000 rpm) with water coolant. Groove-like bone defects were created (85 mJ/pulse, 20 Hz) for histological analysis and evaluation of bone repair ratio. The healing process was evaluated using in vivo micro-computed tomography (micro-CT) every 2 weeks until 8 weeks post-surgery. Sections from bone tissues were created at 24 hours, and 4 and 8 weeks after surgery. Rectangular bone defects were also created (127 mJ/pulse, 20 Hz) to evaluate gene expressions in the bone tissues. Microarray analysis at 6, 24, and 72 hours after bone ablation and quantitative polymerase chair reaction (qPCR) were performed.
Results: Er:YAG laser could effectively ablate bone tissue without major thermal changes. Laser-irradiated sites showed significantly higher bone repair ratios than bur-drilled sites at 2, 4, 6, and 8 weeks. At 6 hours, only 10 differentially expressed genes (DEGs), including SOST, were identified between bur-drilled and laser-ablated bones. The gene expression pattern was clearly different at 24 hours after bone ablation between bur-drilled and laser-ablated bones. Gene Set Enrichment Analysis showed inflammation-related gene sets were enriched in the bur-drilled bone at 6 hours, whereas these gene sets were enriched in the laser-ablated bone at 72 hours compared to that of the control bone. No DEGs were identified between bur-drilled and laser-ablated bone at 72 hours. According to the results of the microarray analysis, focus was placed on the SOST, the gene that suppresses bone formation. Surprisingly, SOST expression increased in bur-drilled bone, whereas it was decreased in laser-irradiated bone, compared to the control bone at 6 hours. Immunohistochemistry revealed the signal for sclerostin (coded by SOST) was weaker in laser-ablated bone than that in bur-drilled bone at 24 hours after bone ablation.
Conclusion: This is the first study to comprehensively and sequentially evaluate gene expression in ablated bone tissue following bur drilling and Er:YAG laser irradiation. The results of this study suggest that Er:YAG laser irradiation may produce accelerated early new bone formation in laser-ablated bone through the advantageous responses and stimulate osteocytes in the bone tissue.
Educational Objectives
- Describe the differences of gene expression in bone tissues that have undergone laser ablation and bur drilling.
- Review the bioinformatic method.
- Understand bone healing after Er:YAG laser ablation.
Laser Information: A pulsed Er:YAG laser (DELight, HOYA ConBio, Fremont, Calif., USA) was used, and laser irradiation was performed at an incident angle of approximately 30° to the moistened surface in contact mode under saline solution irrigation. A curved Er:YAG laser contact tip with 600-µm diameter was used for straight line irradiation and a chisel-type contact tip with a rectangular pointed head of 1.40 mm × 0.45 mm dimension was used for area irradiation.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
6:20 PM - 6:30 PM
Sayaka Katagiri, DDS, PhD | Tokyo, Japan - Dr. Eugene Seidner Researrch Grant Recipient
Photobiomodulatory Suppressive Effect of a 910-nm Diode Laser on Periodontal Disease Progression in Mice
Track: Seidner Research Grants Scholar
Audience: All
Background: The diode laser is currently used for various treatments. However, the effect of diode laser irradiation on bacteria remains unclear. The aim of this study was to investigate the suppressive effect of diode laser irradiation on periodontal disease progression by using ligature-induced periodontitis in mice.
Materials and Methods: Wild type male C57BL/6J mice (9-week-old) were used for experiments. Gingival inflammation and loss of alveolar bone were induced by ligation of 6-0 silk ligature to the maxillary right second molar teeth in mice. A diode laser (Lumix 2™, Fisioline S.r.l., Borgato Molino, Italy) (wavelength: 910 nm) was used at 0.2 W and 30 kHz for 7.5 minutes (total energy: 90 J) at a distance of 1 mm only on the right side, not on the left side, on 1, 3, and 5 days after ligation. In vivo micro computed tomography (CT) imaging was employed before ligation and at 8 days after ligation. DNA was extracted from both laser-irradiated and non-irradiated ligatures at 8 days after ligation. After purification and generation of the multiplexed amplicon library, paired-end sequences (250 bp) were produced by the Illumina Miseq platform. Taxonomic classification of the sequences at the phylum, family, and genus levels were carried out against the GreenGenes database. Gingival tissue was taken from around the maxillary second molars at 3 days after ligation and homogenized. Total RNA was extracted from the excised gingival tissue, and quantitative polymerase chain reaction (qPCR) was performed.
Results: In vivo micro CT analysis revealed that ligation induced severe bone loss. Ligated mice irradiated by diode laser showed suppression of bone loss at 8 days after ligation. Extracted amount of DNA from the ligated ligature was decreased in the diode laser-irradiated mice compared to that in non-irradiated mice. The diversity and composition of microbiome showed no significant difference between laser-irradiated and non-irradiated ligatures. However, different microbiome compositions between the control and laser-irradiated ligatures were observed. mRNA expression in TIMP1, SPP1, and S100A8 were changed after laser irradiation.
Conclusion: This is the first study to comprehensively evaluate the anti-microbial effect of diode laser by using a next generation sequencer. The results of this study suggest that diode laser irradiation may exert an antimicrobial effect and suppress periodontal bone loss. Novel and effective periodontal treatment with photobiomodulation will be developed.
Educational Objectives
- Understand the effect of diode laser irradiation on periodontal disease progression by using ligature-induced periodontitis.
- Review the bioinformatic method.
- Relate the differences in the microbiome on ligature-induced periodontitis between laser irradiation and non-laser irradiation.
Laser Information: Lumix 2 diode laser (Fisioline S.r.l., Borgato Molino, Italy), 910-nm wavelength, was irradiated at 0.2 W and 30 kHz for 7.5 minutes (total energy: 90 J) at a distance of 1 mm
|
 |
6:30 PM - 6:40 PM
Marcos Garcia, DDS | Houston, Texas, USA - Dr. Eugene Seidner Research Grant Recipient
Clinical Outcomes of Adjunctive Antimicrobial Photodynamic Therapy in the Nonsurgical Treatment of Peri-Implant Disease
Track: Seidner Research Grant Scholar | Houston, Texas, USA
Audience: All
Peri-implant mucositis and peri-implantitis are caused by the development and accumulation of a bacteria biofilm around the implant, leading to a shift in bacterial species as the disease progresses. Biofilm-induced peri-implant mucositis is reversible by the removal of plaque from around the implant. The gold standard of care is the mechanical removal of plaque with the use of curettes and ultrasonics. Conventional mechanical debridement of the implant surface is limited by the contaminated microstructure of the implant surface. Options of antimicrobial adjunct treatment of peri-implant inflammation include systemic antibiotics, local antibiotics, antiseptics, and laser therapy such as antimicrobial photodynamic therapy (aPDT). The advantages of aPDT are its wide antimicrobial activity, multiple applications without the risk of resistance, and the ease of its delivery to the implant surface. The null hypothesis of this investigation was that aPDT, as an adjunct treatment to mechanical debridement, will not improve clinical outcomes when compared to mechanical debridement alone. This randomized, double-blinded, controlled clinical study was designed to assess clinical improvements of aPDT as an adjunct to the gold standard of mechanical debridement in the treatment of peri-implant diseases. Thiry-four patients were recruited. Patients were randomly assigned to control (CG) or experimental groups (EG). Patients assigned to CG received traditional nonsurgical mechanical debridement with sham aPDT, and those assigned to EG received traditional nonsurgical mechanical debridement with aPDT. A 660-nm diode laser (Sirona SIROLaser Advance Plus, Dentsply Sirona, Charlotte, N.C., USA) with parameters of 10 J, 100 mW, and 100 seconds, along with a photosensitizer (methylene blue: 0.1 mg/ml) were used. Clinical measurements such as bleeding on probing, pocket depth, plaque, and clinical attachment were collected at baseline, 6 and 12 weeks after treatment. Data was analyzed with 95% confidence interval (P < 0.05).
Educational Objectives
- Explain peri-implant mucositis and peri-implantitis.
- Define antimicrobial photodynamic therapy (aPDT) and summarize its mechanism of action.
- List the advantages of aPDT in the treatment of peri-implant mucositis and peri-implantitis.
Laser Information: 660-nm Sirona SIROLaser Advance Plus (Dentsply Sirona, Charlotte, N.C., USA.) diode laser, energy density of 10 J/site, 100 mW power, duration of irradiation 100 seconds
|
 |
6:40 PM - 6:50 PM
Edmond Rexha, DDSm Stony Brook School of Dental Medicine | Stony Brook, New York, USA
Dr. Eugene Seidner Scholarship Recipient
Peri-Implant Defect Morphology and Temperature Changes During Er,Cr:YSGG-Laser Decontamination
Track: Seidner Student Scholar
Audience: All
Objectives: The architecture of the peri-implant defect may affect how residual heat associated with laser irradiation is disseminated. The aim of this study was to assess the influence of intrabony defect morphology on temperature change (ΔT) of irradiated implants using an Er,Cr:YSGG laser.
Materials and Methods: Five separate defects (circumferential, one-walled, two-walled, three-walled, or horizontal defect) were created around dental implants that were placed into a synthetic (bovine) bone analog that mimics type II quality bone. Each implant surface and the surrounding bone were irradiated by a noncontact, free-running pulsed, 2780-nm Er,Cr:YSGG laser (Waterlase MD, Biolase, Irvine, Calif., USA) at 2 W power for 30 and 60 seconds. Apical and coronal thermocouples placed in contact with the implants were used to evaluate ΔT at 30 and 60 seconds. Statistical comparison was performed using statistical software. The means of (ΔT) during irradiation were compared between the five experimental groups using ANOVA 3/3 models.
Results: The most substantial temperature differences of the coronal and apical thermocouple were observed in the 2- and 3-wall defects as follows: 2-wall defect ΔT (at 30 s 2.88 ± 0.35°C coronal and 2.27 ± 0.20 apical; at 60 s 3.58 ± 0.41 coronal and 2.65 ± 0.16 apical); 3-wall defect ΔT (at 30 s 2.89 ± 0.43 coronal and 2.29 ± 0.36 apical; at 60 s 3.59 ± 0.45 coronal and 2.85 ± .65 apical); circumferential, one-wall and horizontal defects ΔT (at 30 s 0.91 ± 0.16, 2.37 ± 0.37, 0.64 ± 0.32 coronal and 0.37 ± 0.21, 1.17 ± 0.24, 0.21 ± 0.17 apical; at 60 s 1.69 ± 0.30, 3.06 ± 0.25, 1.11 ± 0.37 coronal and 0.73 ± 0.20, 1.96± 0.29, 0.51 ± 0.20 apical), respectively. All test values were shown to be statistically significant (p < 0.0001).
Conclusions: The morphology of the peri-implant defect may affect the resultant heat dissemination of Er,Cr:YSGG laser irradiation on implants. Although none of the defects resulted in a temperature change greater than the 10°C threshold, circumferential, two- and three-walled defects may have a greater risk for overheating and therefore irradiation should be kept within a 30-second period.
Educational Objectives
- Assess the influence of intrabony defect morphology on temperature change (ΔT) of irradiated implants using an Er,Cr:YSGG laser.
- Determine whether there are specific safety settings or protocols that can be established based on temperature change.
|
 |
6:50 PM - 7:00 PM
Wenbin Feng, BS, Touro College of Dental Medicine | Hawthorne, NY
Dr. Eugene Seidner Scholarship Recipient
In Vitro Comparison of Traditional vs. Er,Cr:YSGG Laser Techniques for Interproximal Reduction in Orthodontics
Track: Seidner Student Scholar
Audience: All
Introduction: Interproximal reduction (IPR), slenderization, or reproximation is utilized in orthodontic treatment to gain space to relieve mild-to-moderate dental crowding and to adjust from the Bolton Discrepancy [1]. IPR is the mechanical removal and recontouring of interproximal enamel surfaces. It can be utilized to create up to 8 mm of space in a dental arch [2]. There are several enamel reshaping methods. Commonly used instruments include thin metal abrasive strips, rotary diamond discs, burs, handpiece-mounted oscillating strips and segment discs. Each of these methods has its advantages and disadvantages.
Objective: The aim of this study was to evaluate the efficacy of using an erbium laser in IPR.
Materials and Methods: Fifty-four human teeth were set in stone in groups of six each (five interproximal surfaces per set). Setups included three sets of maxillary anterior teeth, three sets of mandibular anterior teeth and three sets of biscupids. Each of these setups was randomly assigned to one of three groups (n = 9). All areas were prepared to 0.3 mm of reduction, as measured with leaf gauges (Komet USA, Rock Hill, S.C., USA). IPR for Group 1, the control group, was treated with only diamond interproximal sanding strips (Dentsply, York, Pa., USA). IPR was completed in Group 2 using only an Er,Cr:YSGG dental laser (Waterlase iPlus, Biolase, Foothill Ranch, Calif., USA). Teeth in Group 3 were also reduced with an Er,Cr:YSSG dental laser and then followed up with a diamond interproximal sanding strip. One tooth (two interproximal surfaces) were randomly selected from each of the three groups. The enamel surface morphology was to be analyzed by scanning electron microscopy (SEM) analysis, but has not been completed because of Covid restrictions.
Results: Reported results include total procedure time, laser parameters, and comparison of finished surface texture. While the time difference between the erbium laser IPR vs. using a sanding strip only was significant (p≤0.005), there was no significant difference between the time it took to use the erbium laser vs. using the laser followed by a sanding strip (p=0.4). The difference in time between using only a sanding strip alone vs. laser plus sanding strip was significant (p≤0.0005). There was no significant difference between the number of strokes while using the sanding strips, whether or not it was done with or without the laser. Finally, the difference in preparation time between using a new or used laser tip was not significant.
Conclusion: This project demonstrates that the usage of Er,Cr:YSSG laser energy in conjunction with thin metal polishing strips likely achieves an identical surface smoothness as metal abrasive strips alone, while taking less time and providing a safe method for IPR. We can conclude that performing IPR using an erbium laser alone or erbium laser followed by a sanding strip, the total time is significantly shorter than the conventional method of using a sanding strip alone. The difference between using an erbium laser alone and combining erbium laser with a sanding strip was not significant. Erbium lasers could be a viable treatment modality in IPR procedures.
References
1. Lapenaite E, Lopatiene K. Interproximal enamel reduction as a part of orthodontic treatment. Stomatologija 2014;16(1):19-24.
2. Pindoria J., Fleming PS, Sharma PK. Inter-proximal enamel reduction in contemporary orthodontics. Br Dent J 2016;221(12):757-763.
Educational Objectives
- Evaluate the efficacy of using an Er,Cr:YSGG laser in orthodontic interproximal reduction (IPR).
- Develop a protocol that is effective for using an Er,Cr:YSGG laser for IPR and could achieve optimum results.
|
 |
6:30 PM - 7:00 PM
John J. Graeber, DMD, MAGD, MALD, FICD | East Hanover, New Jersey, USA
Finding Virgin Caries
Track: General Dentistry
Audience: All
With the introduction of new techniques and materials into dental practice, the potential of ultraconservative cavity preparation can become a reality. For preserving the maximum of natural tooth structure, the long-held concepts of diagnosis and caries management must change. The use of hundred- or thousand-year-old instrumentation must be replaced with ultrasensitive diagnostic instrumentation. The earliest possible diagnosis and contemporary caries management must replace antiquated X-rays and explorers as well as the “Drill and Fill” mentality. The 70-year-old Air Rotor is responsible for much of the iatrogenic damage to our patients’ teeth. Today’s treatment technology with all-tissue lasers and/or air-abrasive techniques can be utilized to create true micro-invasive treatment with very little need for local anesthetics or rotary instrumentation. These technologies have proven incapable of causing the microfractures leading to tooth fracture or early restoration failure. This presentation will demonstrate current diagnostic and treatment techniques for the patient-oriented practitioner.
Educational Objectives
- Observe micro-videos of actual cavity preparation treatment techniques.
- Incorporate many of these concepts into one’s own dental practice.
- Comprehend the advantages of each diagnostic and treatment device.
|
 |
7:00 PM - 7:30 PM
Charles Hoopingarner, DDS, FAGD, MALD | Austin, Texas, USA
Lasers and Labs: Your Best Friends in Esthetic Dentistry
Track: General Dentistry
Audience: All
Making your patients thrilled with their smile is a team effort with communication being the critical factor. Learning to listen to the patient is paramount. Communication with the laboratory allows all three participants in the experience to work together to achieve the desired result. Principles of smile design should be explained during the interview process. Soft tissue profile is exceedingly important and does not have to be a limiting factor. Soft and hard tissue repositioning can easily and healthily be accomplished with a variety of lasers. Principles of biologic width must be followed to achieve the desired long-term healthy result. Even with meticulous care it is on rare occasion necessary to remove or reposition a final restoration. Laser technology allows this to be done without inconvenience to the patient. Following the principles of team effort outlined in this presentation will allow dentists to produce the consistent, satisfying results that all members of the equation are seeking.
Educational Objectives
- Identify the patient’s objectives.
- Achieve a smile design that meets the patient’s objectives and communicate this information to the laboratory with written and visual instructions.
- Design and achieve a soft tissue framework that complements the patient’s smile with various lasers while maintaining optimum soft tissue health.
- Remove a previously placed restoration and reseat it using a laser.
Laser Information: Soft issue surgeries were done with either a 940-nm diode laser (Biolase, Foothill Ranch, Calif., USA) at 1 Watt and 20% duty cycle or an 810-nm diode laser (Picasso, AMD Lasers, West Jordan, Utah, USA) at 1 Watt and 50% duty cycle. Osseous surgeries were performed with a 2780-nm Er,Cr:YSGG laser (Biolase) at 2-4 Watts with heavy water accompaniment. One combined case was done with a 2940-nm Er:YAG laser (HOYA ConBio, Fremont, Calif., USA) at 1.5 Watts with heavy water usage.
|
| FRIDAY, APRIL 9, 2021 |
 |
9:15 AM - 10:00 AM
Giovanni Olivi, MD, DDS | Rome, Italy
Innovative Endodontics Using SWEEPS: An Update
Track: New Techniques and Technology - Endodontics
Audience: All
Photoacoustic technology is used to activate the commonly used irrigants in endodontics (sodium hypochlorite (NaOCl) and ethylenediaminetetraacetic acid (EDTA)) and does not replace any conventional instrumentation, but only reduces it to a minimal ISO 20-25/04 enlarging of the root end. The initial Photon-Induced Photoacoustic Streaming (PIPS) protocol, and today’s Shock Wave Enhanced Emission Photoacoustic Streaming (SWEEPS) protocols are validated by a wide body of published and non-published experiments and data. Scanning electron microscopy, confocal analysis, and computed tomographic (CT) imaging are used to evaluate tissue dissolution, debridement, smear layer, and endodontic filling material removal from the endodontic space. Bacteriological studies are performed to assess the decontaminating effect of these techniques. High-speed videos at 100,000 frames per second are shown to explain the innovative dual-pulse laser emission in the endodontic environment. The lecture will present an overview of the scientific concepts behind the clinical application and a series of clinical cases.
Educational Objectives
- Know and discuss the limitations of the conventional use of lasers in endodontics.
- Identify the evidence-based literature on photoacoustic techniques in endodontics.
- Specify the advantages of SWEEPS technique in endodontics.
- Enumerate the tips and tricks for efficient and safe use of the laser in endodontics.
Laser Information: 2940-nm Er:YAG laser (LightWalker AT, Fotona, Ljubljana, Slovenia), 20 W maximum output power, free-running pulse, 25-microsecond pulse duration, 15-20 Hz, 10-20 mJ, 400-micron flat-end and radial-end tips. 30 s activation plus resting phase repeated many times during the treatment.
|
 |
10:00 AM - 11:00 AM
Lawrence Kotlow, DDS | Albany, New York, USA
A Retrospective Synopsis of ALD's 2021 Winter Pediatric Health Symposium
Track: Pedodontics
Audience: All
This past winter the Academy of Laser Dentistry presented a 10-week continuing education symposium on the tongue and airway. A group of internationally recognized authorities presented their expertise on the near- and long-term effects of restrictive tethered oral tissues (RTOTs). The aim of this presentation is to provide a glimpse into the importance of early intervention and the interdisciplinary team approach to early care and how we as clinicians can make a positive difference in the lives of so many people. A summary of the following topics will be covered. The full symposium is available on-demand throughout 2021.
- Pediatric dysfunction
- Cranial development
- Myofunctional therapy and maternal bonding
- Orthodontics and the tongue
- The tongue as it relates to the airway
- Chiropractic care of the infant with TOTs
- Pre- and post-frenectomy therapy for speech development
- Laser therapy for airway management
- Managing bleeding during TOTs care
- Insurance and medical reimbursement
Educational Objectives
- Explain how restrictive ankyloglossia can affect long-term brain development and contribute to orofacial myofunctional disorder.
- Identify the members of the assessment and treatment team for RTOTs.
- Discover how to do a proper assessment and examination to determine the existence of RTOTs.
- Summarize available treatment solutions for tethered oral tissues.
|
 |
11:00 AM - 11:45 AM
Jeffrey Harrison, DDS | Cortez, Colorado, USA
Dental Management of Obstructive Sleep Apnea
Track: New Techniques and Technology - Sleep Apnea
Audience: All
While COVID-19 may be the most important pandemic on everyone’s mind, the most important epidemic facing your patients is getting far less attention and causing far more harm – obstructive sleep apnea (OSA). One in four of the adult patients you saw today is already starting to suffer from this not-so-silent killer without their knowledge. Medicine has failed to adequately identify and treat most patients in need and now dentists find themselves being asked to serve on the front line for screening, diagnosing these patients, and possibly playing an important role in their management. Make 2021 the year you stop ignoring the dental warning signs and start to collaborate with other health care providers by understanding the connection airway, sleep, and breathing has with the dentistry you are doing every day.
Educational Objectives
- Enumerate the signs and symptoms of sleep-related breathing disorders.
- Appreciate the prevalence of the obstructive sleep apnea epidemic.
- Learn a patient- and physician-friendly protocol to follow from screening through diagnosis, treatment, and medical insurance reimbursement.
- Specify where to go next for education and training.
Product Information: EccoVision Pharyngometer / Rhinometer (Sleep Group Solutions, Hollywood, Fla., USA).
|
 |
11:45 AM - 12:45 PM
Moderator: Rishita Jaju, DMD | Reston, Virginia, USA
Panelists: Jeffrey Harrison, BA, DDS; Lawrence Kotlow, DDS; Giovanni Olivi, MD, DDS
( LIVE ) Panel Discussion: Question-and-Answer Session
Track: New Techniques and Technology
Audience: All
New techniques and technologies in laser dentistry are an exciting topic for all new and experienced dental laser practitioners. Applications in endodontics and pediatric dental treatment and management of obstructive sleep apnea will be reviewed with experience, expertise, and best literature evidence available.
Educational Objectives:
- Summarize the application of Shock Wave Enhanced Emission Photoacoustic Streaming (SWEEPS) technology for endodontic treatment.
- Review the steps in preparing the office for treatment of patients with restrictive tethered oral tissues (RTOTs).
- Discuss dental management of sleep apnea.
- Identify benefits, limitations, and potential risks of new applications in each field.
|
 |
12:45 PM - 1:30 PM
V. Kim Kutsch, DMD
Dental Aerosols: Air Safety in Dental Offices
Track: Covid-19
Audience: Novice
Dental professionals are routinely exposed to aerosols generated by a variety of dental instruments. These aerosols contain potential pathogens and represent serious health risks to the professional. The high-speed turbine handpiece is the most obvious aerosol generator, but other instruments like sonic and ultrasonic scalers, hard tissue lasers, and even the air-water syringe also contribute significant aerosols. To address the risks from these aerosols, dentistry has adapted universal precautions for infection control and personal protective equipment (PPE) recommendations. In light of the COVID-19 pandemic, current PPE recommendations include an appropriate rated respirator or mask for the procedure, face shield, head cap, gown, gloves, and shoe coverings to reduce the exposure and potential spread of infectious diseases. These help to protect the professional from exposure, but do nothing to minimize the potential pathogenicity or control of the origin of the aerosol during the procedures. This program will present strategies to reduce the health risk of the dental aerosol with preprocedural rinses and also to control the aerosol with extraoral vacuums.
Educational Objectives
- Discuss the health risks of dental aerosols for dental professionals.
- Examine recommended measures and additional strategies to reduce disease transmission from dental aerosols.
- Implement simple universal dental aerosol strategies.
Product Information: 99.99% high-efficiency particulate (HEPA) extraoral vacuum (DAX, Dental Safety First, Albany, Ore., USA); Carifree preprocedural rinse (0.20% sodium hypochlorite) (Oral BioTech, Albany, Ore., USA)
*Sponsored by CariFree
|
 |
1:00 PM - 2:00 PM
Walid Altayeb, DDS, MScD, PhD | Doha, Qatar
Ideal Clinical Laser Dentistry Using Multiple Diode Laser Wavelengths (450, 650, & 980 nm)
Track: Business of Dentistry
Audience: All
Background: The clinical application of lasers in oral soft-tissue surgery has continued to expand in the last two decades. Diode lasers are becoming quite popular due to economic and ergonomic considerations. Diode wavelengths in the visible spectrum (450 and 650 nm) and in near-infrared spectrum (980 nm) are widely used in dentistry.
Clinical Implications: Diode laser wavelengths are absorbed mainly by hemoglobin and melanin. Differences in their absorption characteristics require amendment of the treatment protocols for each wavelength including the laser settings (energy and exposure duration) and mode of application (contact or noncontact). Soft tissue ablation, disinfection, biostimulation, and hemostasis without causing collateral thermal damage are the desired clinical outcomes and could be achieved by using the appropriate diode wavelengths to target the specific chromophores at various depths in the oral tissues. The 450-nm wavelength has greater absorption in hemoglobin and melanin compared to other infrared wavelengths. This provides an opportunity to achieve tissue ablation using the photothermal effect (noncontact mode) and more efficient coagulation. The 980-nm wavelength has deeper penetration than 450 nm which leads to remarkable disinfection in periodontal diseases. The 650-nm wavelength is one of the optimal wavelengths for photobiomodulation due to its deep penetration and ability to irradiate the deep tissues with relatively low energy that accelerates wound healing and relieves pain.
Conclusion: Understanding the optical properties and absorption characteristics of diode laser wavelengths is the key to achieve the clinical goals without causing collateral thermal damage.
Educational Objectives
- Outline the biologic laser-tissue interaction of different diode laser wavelengths.
- Determine how to select between the different diode wavelengths.
- Employ the absorption characteristics of diode wavelengths to achieve the ideal clinical goals.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
*Sponsored by Wuhan Pioon Technology Co., Ltd
|
 |
1:30 PM - 2:30 PM
Kelly Blodgett, DMD, NMD, IBDM | Portland, Oregon, USA
Predictable Periodontal Payoffs! (A PPP We Can All Support): Combining Lasers and Rx Periodontal Trays for Optimal Clinical Outcomes
Track: Business of Dentistry
Audience: All
Laser therapies have revolutionized our restorative, periodontal, and cosmetic treatments, yet even excellent initial results can break down over time. Combining Rx periodontal trays with laser therapies creates greater patient compliance, makes them an active participant in the improvement of their health, and simplifies the laser treatments you offer. Additionally, Rx periodontal trays can offer an additional revenue stream for your practice which requires zero doctor time or energy.
Educational Objectives
- Relate the benefits and limitations of laser therapy and prescription tray therapy to treat oral infection and inflammation.
- Recognize technologies that multiply your team’s effectiveness and productivity.
- Empower patients to maintain oral health with a patient-centered health model.
*Sponsored by Perio Protect
|
 |
5:00 PM - 5:45 PM
Manaf T. Agha, DDS, MD, PhD | Dubai, United Arrab Emirates
Laser Treatment for Oral Melanin Hyperpigmentation
Track: Esthetic Dentistry
Audience: Both
The normal appearance of the gingiva and lips is pink to light red and this appearance may change due to many factors and might be noticeable causing esthetic concerns. In the Gulf area, melanin pigmentation is a concern for some individuals and patients expect the pigmentation to be removed for esthetic reasons. Many techniques have been used to remove the melanin pigmentation such as using surgical blades, diamond or ceramic burs, chemicals, and lasers. This presentation highlights the use of many laser wavelengths in the treatment of hyperpigmentation. Discussion will include an understanding of the mechanism of different wavelengths in melanin pigmentation removal, and clinical outcome parameters including bleeding, wound healing, pain, duration of procedure, color improvement, patient satisfaction, and relapse.
Educational Objectives
- Relate the causes of oral melanin hyperpigmentation.
- Understand the mechanism of different laser wavelengths in the treatment of melanin hyperpigmentation.
- Recognize the adverse effects and the limitations of different laser wavelengths in melanin depigmentation procedures.
|
|




|
5:00 PM - 5:45 PM
Lynn Atkinson, RDH; Jeanette K. Miranda, RDH, BSDH; Mary Lynn Smith, RDH; Angie Wallace, RDH
Laser Bacterial Reduction (LBR): Fact vs. Fiction
Track: Hygiene
Audience: All
This presentation discusses the information and misinformation surrounding Laser Bacterial Reduction, or LBR. The first segment will provide research to support LBR and anecdotal experience with successful LBR treatment. Technique will be reviewed and the distinction between Laser-Assisted Periodontal Therapy (LAPT) and Laser Bacterial Reduction (LBR) will be examined. The second segment will be open to attendees for a question-and-answer session.
Educational Objectives
- Explore the research on laser bacterial reduction (LBR).
- Differentiate between LBR and LAPT.
- Review technique for LBR.
|
 |
5:45 PM - 6:30 PM
Kristin Pristavec-Hunter, RDH, BS | Dallas, Texas, USA
Innovative Technology: A Review of Current Lasers
Track: Hygiene
Audience: All
Dental practices across the country, and their patients, are enjoying the advantages inherent to laser technology. From early cavity detection to cosmetic treatments, dental lasers are a versatile tool that saves time, lessens discomfort, and dramatically improves the patient experience. If a dentist is considering investing in a laser for the dental practice, an understanding of the different devices on the market and the use of each one is important.
- Pros of laser dentistry: The dental laser is a versatile tool that offers a number of benefits to dentists, hygienists, and patients alike.
- More efficient: The dental laser makes dental procedures themselves faster, with fewer follow-up visits afterward.
- Minimally invasive: In most cases, laser dentistry reduces pain and discomfort for the patient. Because there is less pressure, patients may not need general anesthesia or anesthetic.
- Increased precision: The laser is a very precise tool, allowing a dentist to preserve healthy tissue and tooth material. That makes the laser especially useful for the treatment of dental caries or periodontal disease.
- Reduced patient anxiety: Patients who fear the dental drill will find the laser much less intimidating. These tools are smaller and much quieter, and the reduced pain and discomfort helps patients feel more relaxed during treatment.
- Reduced risk of infection: Because it is a single tool, the dental laser can help keep the area disinfected, reducing the risk of bacterial infections.
- Reduced bleeding and swelling: With little trauma caused to the gum, tooth, and surrounding tissue, laser treatments mean minimal bleeding and much faster recovery times.
- Versatility: Soft-tissue lasers and hard-tissue lasers can be used for a wide variety of dental procedures in adult and pediatric patients.
With so many positive aspects to the laser it is important to understand the differences of the lasers on the market, what they are used for, and the different features they have. Today’s dental lasers can be used in nearly every aspect of dentistry, and for many practices, the advantages clearly outweigh the negatives. Understanding the pros and cons of laser dentistry makes it easier to evaluate how a dental laser might help one’s practice.
Educational Objectives
- Review current dental laser devices on the market.
- Relate their different uses in hard tissue and soft tissue.
- Specify estimates of costs and product features.
Laser Information: Lasers from AMD Lasers, West Jordan, Utah, USA; Biolase, Foothill Ranch, Calif., USA; Convergent Dental, Needham, Mass., USA (Solea); DenMat, Lompoc, Calif., USA (SOL); Dentsply Sirona, Bensheim, Germany; Great Plains Technologies, Fairfield, Neb., USA (Denta II); King Dental, Prospect, Ky., USA (Beamer); Ultradent, South Jordan, Utah, USA (Gemini).
|
 |
6:30 PM - 7:00 PM
Marta Maciak, DMD, PhD | Krakow, Poland
A Concept of Using Various Laser Wavelengths in Effective, Noninvasive Esthetic Medicine
Track: Esthetic Dentistry
Audience: All
Lasers are very popular in conventional esthetic medicine treatment and procedures. However, it is common that mostly ablative and nonablative deeply penetrating wavelengths are recommended. Unfortunately, the methods used often require a long convalescence time, which is uncomfortable for the patients even if the results are mostly predictable. The lecture will introduce a combination of different laser wavelengths in esthetic medicine based on the literature, and knowledge and experience of the lecturer. Photobiomodulation seems to be the future of all kinds of treatment, also in the field of esthetic medicine. Noninvasive skin rejuvenation is a natural way of rejuvenation thanks to collagen stimulation with the use of different laser wavelengths (635, 980, 1064, and 2940 nm) combined with proper cosmetics, which gives the same results as invasive methods but is more accepted by patients. The effects of noninvasive skin rejuvenation are long-lasting thanks to natural stimulation of the patient’s cells involved in the whole procedure; no side effects are observed, which is crucial for the patient. The laser is also very effective for acne treatment. The combination of different wavelengths and photoactive disinfection significantly reduces the number of bacteria even after one session without scars and relapse of the disease. The use of new multiwavelength lasers is now commonplace in dentistry; however, the emergence of new modalities and wavelengths is going to raise the standard of care and esthetic values for our patients.
Educational Objectives
- Gain an understanding of wavelength-specific modalities.
- Describe how to use different laser wavelengths in esthetic medicine.
- Identify properties of a laser in everyday practice.
- Enumerate the advantages of multiwavelength lasers.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
6:30 PM - 7:15 PM
Camille Luke, RDH, MSDH | Tumwater, Washington, USA
You Are Not Alone!
Track: Hygiene
Audience: All
Practicing dentistry during a pandemic has added stress to team members and patients alike. How are you and your team dealing with these issues? What sort of tips and techniques are you employing to help yourself, your co-workers, and your patients? What do you do if a team member tests positive or has been notified they were around someone who tested positive? What seem to be the biggest stressors for your patients? What kinds of questions are they asking your team members? Sit down with us and listen to how a group practice is dealing with these issues. Know that you are not alone in this and learn from the experiences of others.
Educational Objectives
- Identify the 3 key points to reduce stress and keep you focused and positive during a pandemic.
- Recognize scheduling practices to maintain productivity and deliver quality patient care.
- Provide answers for the top 3 questions asked by patients visiting the dental office.
|
 |
7:15 PM - 8:00 PM
Moderator - Angie Wallace, RDH
Panelists - Lynn Atkinson, RDH; Jeanette K. Miranda, RDH, BSDH; Mary Lynn Smith, RDH; Angie Wallace, RDH
Track: Hygiene
Audience: All
We will be discussing and clearing up several concerns and incorrect information that has been published about laser bacterial reduction (LBR). Many times, this procedure is confused with laser-assisted periodontal therapy (LAPT). We will take the time to share with you the difference between the two procedures, some of the studies that have been published, and how to do the LBR procedure. We welcome questions and will discuss how we can make sure we are all on the same page as we present information to our patients.
As we delve into Innovative Technology, we will explore the new information and equipment that is available to Dental Hygienists, and answer your questions on how to get trained in these tools and be able to use them chairside.
Many times we feel overwhelmed and we will help you feel comfortable with the techniques and skills needed to get through some of these tough times in dental hygiene.
The panelists will discuss the possible benefits, limitations, and potential risks of these topics while respecting clinical expertise and best evidence.
Educational Objectives
- Review advantages of Laser Bacterial Reduction in practicing dental hygiene.
- Understand differences in dental lasers available to the dental hygienist.
- Explore the impact of COVID-19 on the practice of dental hygiene.
|
| SATURDAY, APRIL 10, 2021 |
 |
9:30 AM - 10:15 AM
Josep Arnabat-Dominguez, MD, DDS, PhD | Barcelona, Spain
Effect of Photobiomodulation on Long-Standing Neurosensory Alterations of the Inferior Alveolar and Lingual Nerves
Track: Photobiomodulation
Audience: All
Surgical removal of the lower third molar is one of the most common oral surgical procedures. One of the complications that can occur after this type of surgery is the neurosensory alteration of the inferior alveolar nerve (IAN) and lingual nerve. Although it is not the most frequent complication (1.3%), in some cases the complication is considered permanent (0.3%). Different treatments have been proposed to reduce discomfort in patients (vitamin B complex such as vitamin B1, B6 and B12, and anti-inflammatories), but the results are not always satisfactory. The use of photobiomodulation (PBM) has been described to treat long-standing neurosensory alterations of the IAN and is generally accepted due to its minimally invasive approach. This presentation will review published studies relating to these long-standing neurosensory alterations and evaluate and describe the results of photobiomodulation therapy on the treatment of long-standing neurosensory IAN alterations after lower third molar extraction.
Educational Objectives
- Review published studies involving long-standing neurosensory alterations of the inferior alveolar and lingual nerves.
- Discover photobiomodulation treatment in long-standing neurosensory alterations of the inferior alveolar and lingual nerves.
- Summarize results of a case series study using PBM therapy.
Laser Information: An 810-nm semiconductor GaAlAs diode laser, average power of 200 mW, continous mode (CW), energy of 4 J, fluence of 4 J/cm2
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
9:30 AM - 10:15 AM
Rose Nierman, RDH | Tequesta, Florida, USA
Cross-Coding: Incorporating Medical Billing for Laser Dentistry
Track: Business of Dentistry
Audience: All
As dentistry continues to shift toward oral-systemic wellness, more dental procedures are being recognized as medically necessary and being covered under major health insurance plans and policies. Dental practices are recognizing the significant benefits to offering medical insurance reimbursement such as increased case acceptance, expanded referral networks, and increased revenue. Cross-coding practices that utilize the patient’s medical insurance are maximizing the patients’ benefits and giving them easier access to much-needed care. In this lecture, attendees will learn how to incorporate cross-coding and medical billing into their office.
Discussion will include the services that can potentially be covered by medical insurance, including laser procedures such as frenectomies and treatment of mucositis and pain conditions. Also covered will be the requirements for receiving reimbursement and a step-by- step guide for how to get started.
Educational Objectives
- Discover which dental laser procedures can be covered under medical insurance.
- Understand what is needed to bill medical insurance for laser dentistry services.
- Determine how to get started with billing medical insurance in dentistry.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
*Sponsored by Nierman Practice Management
|
 |
10:15 AM - 11:00 AM
Mel A. Burchman, DDS | Pennsylvania, USA
Using Dental Lasers to Treat the Chemotherapy Patient
Track: Photobiomodulation
Audience: All
I have been using lasers to treat medically compromised patients since 1998. It is the most rewarding things I have done in 45 years of practice. In July my wife was diagnosed with localized advanced pancreatic cancer and has been receiving 3 very strong chemotherapy agents including fluorouracil (5FU). This presentation will teach how to use photobiomodulation (PBM) and acupuncture to help manage many of the side effects of chemotherapy treatments. As dentists we think about oral mucositis, but patients also have chemo-related sores in other areas of the body. There are also chemo-related temporomandibular joint (TMJ) problems, a cold and tingling finger symptom, as well as problems with nausea, headaches, and stress. This presentation will cover how I use PBM to treat all of these problems. So if you know someone that is having chemotherapy-related problems and would like to be able to help them, I invite you to attend my presentation.
Educational Objectives
- Describe how to use PBM to treat and prevent oral mucositis.
- Learn how to use PBM and laser acupuncture to control chemo-related nausea, headaches, TMJ problems, and cold and tingling fingers.
Laser Information: Q1000 device with 660 and 808-nm tips and the 470-940 nm cluster head; MedX Home Console laser at 633 and 870 nm; MedX Rehab laser at 808 nm with 470 nm guide light (MedX Health, Mississauga, Ontario, Canada).
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
10:15 AM - 11:00 AM
Ron Kaminer, DDS, FAGD | Hewlett, New York, USA
Technology-Driven Restorative Dentistry
Track: Business of Dentistry - Digital Dentistry
Audience: All
The day-to-day restorative dental practice is filled simplicities and complexities. Having the right technology from a laser perspective and having state-of-the-art materials minimizes the complexities. Join us as we highlight some difficult clinical cases, both from direct and indirect dentistry, and show step-by-step how we solve these case problems with lasers and technology.
Educational Objectives
- Explain how different laser wavelengths can be used in day-to-day practice.
- Realize the advantage of using a point-and-shoot camera in day-to-day dentistry.
- Learn why certain laser wavelengths mesh perfectly with advanced restorative materials.
Laser Information: Dual-wavelength 810- and 980-nm diode laser (Gemini, Ultradent, South Jordan, Utah, USA), 1 Watt superpulsed with 400-micron tip.
*Sponsored by SHOFU
|
 |
11:00 AM - 11:45 AM
Gerald Ross, DDS | Alliston, Ontario, Canada
Photobiomodulation in the Treatment of Facial Pain / TMD
Track: Photobiomodulation
Audience: All
This presentation will discuss anatomy and function of the jaw and facial muscles and a list of the various conditions causing facial pain / temporomandibular dysfunction (TMD) pain. Included is a discussion of treatment and how photobiomodulation therapy (PBMT) can play a major role in successful treatment without the use of pharmaceuticals.
Educational Objectives
- Know the anatomy and function of the stomatognathic system.
- Identify which stomatognathic conditions to treat depending on one’s level of experience.
- Understand the role of PBMT in these treatments.
- Return to your office and begin applying what you have learned.
Laser Information: Multiple laser and light-emitting diode (LED) devices will be shown.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
11:45 AM - 12:15 PM
Grace Sun, DDS, MALD, MAGD, MICOI, FAACD | Los Angeles, California, USA
PBMT at Home
Track: Photobiomodulation
Audience: All
PhotoBioModulation Treatment (PBMT), a term equivalent to Low-Level Laser Therapy (LLLT), is a therapeutic form of red and infrared (IR) light therapy that provides a wide range of therapeutic benefits. Reduction of inflammation, efficient wound healing, faster muscle recovery, increased microcirculation, accelerated lymphatic drainage, and analgesic effects are some of these benefits. PBMT can be an excellent addition to conventional dental procedures and oral surgeries due to the increased efficiency of cellular function when receiving red and IR light therapy. As diode technology has advanced in recent years, the benefits of PBMT are now available in both professional treatment facilities as well as at home. Dentists are the bridge between these two worlds. This lecture covers new concepts in red and infrared light therapy and the vital role dentists play in administering this treatment.
Educational Objectives
- Review the benefits of PBMT.
- Explore LLLT, PBMT, laser devices, and light-emitting diode (LED) devices.
- Discuss protocols for PBMT at home.
Laser Information: 2 LED light therapy devices with the following wavelength sets:
- PBM Light: 630 nm, 660 nm, and 850 nm
- PBM Light +: 660 nm, 850 nm, and 940 nm
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
|

|
11:00 AM - 11:30 AM
Edward R. Kusek, DDS | Sioux Falls, South Dakota, USA
Clinical Photography with Use of the Shofu EyeSpecial C-III
Track: Demonstration Course - Photography
Audience: All
The course will demonstrate how to take a variety of photographic images with the Shofu EyeSpecial C-III cameras that meet the guidelines of the American Academy of Cosmetic Dentistry (AACD).
VIEWS
Non-Retracted Views
- Natural full face – formal view – 1:10 (1:15) magnification
- Full natural smile – frontal view – 1:2 (1:3) magnification
- Full natural smile – right lateral view – 1:2 (1:3) magnification
- Full natural smile – left lateral view – 1:2 (1:3) magnification
Retracted Views
- Upper and lower teeth slightly parted – frontal view – 1:2 (1:3) magnification
- Upper and lower teeth slightly parted – right lateral view – 1:2 (1:3) magnification
- Upper and lower teeth slightly parted – left lateral view – 1:2 (1:3) magnification
- Maxillary anterior in view only – frontal view – 1:1 (1:5) magnification
- Maxillary anterior in view only – right lateral view – 1:1 (1:5) magnification
- Maxillary anterior in view only – left lateral view – 1:1 (1:5) magnification
Retracted Views Using a Mirror
- Maxillary arch – occlusal view – 1:2 (1:3) magnification
- Mandibular arch – occlusal view – 1:2 (1:3) magnification
The course will discuss how to use the camera to aid in communication with dental laboratories, how to take surgical pictures quickly, and the limitations of the camera. Included is a video presentation on how to set up the shot and show a perfect shot from each of the situations. The course will also discuss use of aids to best attain near-perfect pictures by any auxiliary.
Educational Objectives
- Learn how to take photos appropriate for AACD presentation.
- Discover tips for shade matching.
- Identify special tips and tricks for successful clinical photography.
Product Information: Shofu EyeSpecial C-III camera
*Sponsored by SHOFU
|
 |
12:15 PM - 12:45 PM
Maite Moreno, DDS, MS | Tijuana, Mexico
State of the Art and Future of Laser-Assisted Oral Mesenchymal Stem Cells and Their Application in Dental and Medical Conditions for Tissue Engineering
Track: Photobiomodulation
Audience: All
Oral mesenchymal stem cells are a new emerging technology that dentists may use in regenerative medicine and dentistry. Medical and dental practitioners are including oral stem cells as a biomaterial in their practices, since they understand the improvement in general health and dental regenerative procedures that can result. The learning curve in tissue engineering is intricate due to the different stem cells in the oral cavity. This lecture will review the main laser-assisted protocols in pulp stem cells and in gingival stem cells. Multidisciplinary attention to the treatment of patients using oral stem cells will require specialized medical doctors and specialized dentists working together as a vanguard professional team in new therapeutical regenerative procedures in dentistry and medicine.
Educational Objectives:
- Understand that laser-assisted mesenchymal stem cells is an emerging technology that will impact tissue engineering, organ engineering, and regenerative medicine and dentistry.
- Learn how laser-assisted pulp stem cells have been used in human trials along with the dual application of laser-assisted gingival stem cells in medical and dental conditions.
- Identify different laser wavelengths and parameters used in pulp stem cell and gingival stem cell research.
Laser Information: 904-nm infrared laser (kTV, Lasertech, San Luis Tlatilco, Naucalpan de Juárez, State of Mexico, Mexico), Class 3B, 500 mW, 180-ns pulse width, 500-4000 Hz, 3-mm diameter tip.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
12:00 PM.- 12:30 PM
Hans Kristian Skjorshammer, BSc | Sun Dental Group, Los Angeles, California
A Win-Win Business Model with PBMT
Track: Photobiomodulation
Audience: All
This session lays out a new method that practitioners can easily institute in their practice to generate new revenue streams while facilitating patient care both in and out of the dental practice. The benefits of PhotoBioModulation Therapy (PBMT) have regained popularity in recent years. Maturation of light-emitting diode (LED) technology has enabled Oral IQ to introduce an affordable home care unit that is portable, compact, economical, user-friendly, and safe with its unique combination of red and near-infrared wavelengths to be used for PBM therapy. Oral IQ’s new medical graded home light treatment units, PBM Light and PBM Light +, and its business model are designed for medical professionals and health practitioners seeking to spread the benefits of PBMT from clinical settings into the home. PBM Light is the ideal solution for treating postoperative surgery pain and discomfort, speeding up healing and recovery in between doctor’s visits, and managing pain relief from the convenience of one’s home, in clinic, and on the go. It allows medical professionals to build a relationship with their patients and extend their service beyond in-house treatment to reach their patient’s home care program. With PBM Light, a sustainable business model is established, via direct dispensing or the Oral IQ affiliate program, providing a win-win situation for both patients and practitioners.
Laser Information: Both Oral IQ LED light therapy devices are FDA Class 2 registered medical-grade devices with the following wavelength sets:
- PBM Light: 630 nm, 660 nm, 850 nm
- PBM Light +: 660 nm, 850 nm, 940 nm
Educational Objectives
- Learn a win-win business model with PBMT.
- Service patient needs beyond the clinical setting through (1) direct dispensing and (2) the Oral IQ affiliate program.
- Comprehend how the PBMT treatment modality is ideal to service patient needs beyond the clinical setting.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
*Sponsored by Oral IQ
|
 |
12:45 PM-1:15 PM
Arun A. Darbar, BDS, DGDP(UK) | Leighton Buzzard, Bedfordshire, United Kingdom
Prevention and Management of Orofacial Muscle Fatigue
Track: Photobiomodulation
Audience: Both
Patients attending our practices for long sessions are always apprehensive that they may not be able to cope with or help us by trying to keep their mouth open wide enough for us to complete their treatment efficiently. The reasons for this can range from strong to weak musculature, jaw joint problems, fear of gagging, and other compliance issues. Needless to mention, our dentofacial structures are one of the very personal and crucial parts of our bodies. Speech, smell, expressions, and breathing are a few of the finer sensitivities involved. Professionally we work within this area which is not always easy or a pleasant experience for our patients, hence anything we do to help goes a long way in patient care and maintenance. Dental professionals can help prevent and manage possible related treatment complications fairly easily and effectively with photobiomodulation therapy (PBMT).
Educational Objectives
- Understand the mechanisms of muscle fatigue.
- Manage patient anxiety and prevent postoperative complications with proactive treatment management.
- Manage muscle relaxation during dental procedures with PBMT and other modalities.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
1:15 PM-1:45 PM
Christopher Walinski, DDS | Valhalla, New York, USA
What I Did on My COVID Break
Track: Photobiomodulation - Covid-19
Audience: All
The coronavirus pandemic has affected each of us in a different way. As an educator, I knew early on that my face-to-face teaching would come to an end or at least be suspended, as more businesses and “non-essential” health care facilities were ordered to close. What to do? I made the decision to accept the situation as a gift, and as with any gift, I did not want to waste it. I decided that when the shutdown ended, there would be deep regret if the gift of time had not been utilized wisely. The results of the COVID break will be presented, including a brief discussion of multiple peer-reviewed research papers. The intent is to inspire others to do the same, should another global shutdown be in our future. The studies to be discussed are in the areas of photobiomodulation therapy (PBMT) in the management of temporomandibular disorder (TMD) symptoms, the immunomodulatory activity in fibroblasts as a result of PBMT, resin cement removal from titanium dental implants, measuring speed and pulpal temperature during Class II cavity preparation using an erbium laser, comparing composite removal using a high-speed handpiece vs. erbium laser, and guidelines for soft tissue laser biopsy.
Educational Objectives
- Discuss the effects of various laser fiber shapes (end-firing, side-firing, and radial-firing) on periodontally involved root surfaces.
- Learn whether to increase the energy per pulse or pulses per second in order to optimize speed while maintaining safe pulpal temperature during laser cavity preparation.
- Specify the ideal parameters to debride and decontaminate ailing titanium implants with an erbium laser.
Laser Information: The lasers used in the studies to be presented include the THOR laser (THOR Photomedicine, Chesham, Buckinghamshire, United Kingdom), OraLase (MedX Cold Laser Technologies, Mississauga, Ontario, Canada), Gemini (Ultradent Products, South Jordan, Utah, USA), and Waterlase iPlus (Biolase, Foothill Ranch, Calif., USA).
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
2:30 PM-3:00 PM
Jason Pang, BSc, BDS, MSc | Sydney, New South Wales, Australia
1064-nm Nd:YAG as a Novel Wavelength for the Treatment of Oral Mucositis
Track: Photobiomodulation
Audience: All
Oral mucositis (OM) is a painful and debilitating side effect of cancer therapy that affects a large proportion of cancer patients. It remains a significant treatment-related toxicity with no assured means of prevention. Through the work of many researchers, clinical trials, systematic reviews, and meta-analyses, light therapy known as photobiomodulation (PBM) has been recommended by the National Institute for Health and Care Excellence (NICE) and the Multinational Association of Supportive Care in Cancer / International Society of Oral Oncology (MASCC/ISOO) for the prevention of OM and related pain. It can improve a broad range of complications, and has an important role in supportive care. The therapy is atraumatic, well tolerated, with minimal side effects. The effective dosimetry has been reduced to a narrow range but is still not effective in all cases. Individual variation and multiple treatment parameters continue to complicate effective management. The 1064-nm Nd:YAG laser is a wavelength commonly used by dentists. More recently it has been used for PBM to treat a range of orofacial pain conditions and to improve wound healing. Using a prototype collimated flat-top profile handpiece, it was possible to simplify the PBM treatment of an oral mucositis patient. Reduced treatment time, ease of treatment and easier access to the nasopharynx were distinct advantages. In the first reported use of a 1064-nm Nd:YAG laser with a prototype handpiece for OM, results were similar to accepted PBM OM protocols and there were no complications or side effects. Rapid healing of ulceration was observed.
Overall, Nd:YAG PBM therapy prevented the need for parenteral nutrition and allowed for uninterrupted continuity of cancer therapy. The 1064-nm Nd:YAG laser should be investigated as a potential wavelength for the treatment of OM.
Educational Objectives
- Appreciate that oral mucositis (OM) is a painful and debilitating side effect of cancer therapy that affects a large proportion of cancer patients.
- Learn that photobiomodulation (PBM) is the recommended treatment for the management of OM and related pain, and has an important role in supportive care.
- Discover that the 1064-nm Nd:YAG laser is a novel wavelength for the treatment of OM, with reported results that were similar to accepted PBM OM protocols without complications or side effects.
Laser Information: THOR Photomedicine LX2 (THOR Photobiomedicine, Chesham, Buckinghamshire, United Kingdom) with 69-diode LED cluster handpiece (34 x 660 nm and 35 x 850 nm diodes), 50 mW/cm2, 2.5 Hz, 60 s, 3 J/cm2.
PIOON S1 (PIOON, Hubei, China), 650-nm laser, 100 mW/cm2, 2.5 Hz, 60 s, ~4 J/cm2.
LightWalker ATS (Fotona, Ljubljana, Slovenia), 1064-nm Nd:YAG laser with prototype flat-top handpiece, 0.5 W/cm2, 10 Hz, 60 s, 100-µs pulse duration, 30 J/cm2.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
 |
3:00 PM - 4:00 PM
Panel Discussion: Question-and-Answer Session: Photobiomodulation
Moderator - James Carroll, AMInstP, FRSM
Panelists - Josep Arnabat-Dominguez, MD, DDS, PhD; Mel A. Burchman, DDS; Maite Moreno, DDS, MS; Jason Pang, BSc, BDS, MSc; Gerald Ross, DDS; Grace Sun, DDS, MALD, MAGD, MICOI, FAACD; Christopher Walinski, DDS
Track: Photobiomodulation
Audience: All
Photobiomodulation (PBM) is a therapeutic light-based agent that stimulates faster and better tissue repair, reduces inflammation, reduces edema, and induces an analgesic effect. Widely used in musculoskeletal pathologies, PBM is emerging as a potential important adjunctive therapy in dentistry. For example: treatment of postoperative tissue trauma reduces the need for opioids or anti-inflammatory medication; improved neurosensory recovery after long-standing injury to the inferior alveolar nerve is routinely achieved; dentine hypersensitivity is reduced almost instantly and maintained for months after a single treatment; chronic temporomandibular disorder (TMD) is relieved where occlusal splints and medication have no beneficial effect. This session is an opportunity to ask the panel anything about PBM. They are experienced clinicians and academics on all aspects of PBM including mechanisms of action, physiological changes, clinical benefits, research evidence, treatment parameters, dose, safety, side effects, treatment reactions, contraindications, U.S. Food and Drug Administration (FDA), American Dental Association (ADA) policy, reimbursement, business and marketing matters.
Educational Objectives
- Address audience questions on PBM safety, efficacy, and legal matters.
- Learn how to add PBM to your business effectively.
Note: This presentation discusses investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.
|
EVENT SPONSORS
Click here for sponsorship opportunities
SPONSORSHIP PACKAGES
Click here for sponsorship package descriptions.
ALD Organization Disclosure - Disclaimer on Protocols and Opinions
The views expressed and opinions and materials presented during a presentation represent the personal views and opinions of the individual speakers and do not necessarily represent the views and opinions of the Academy of Laser Dentistry. The Academy of Laser Dentistry assumes no responsibility for the content of the presentations made by individual speakers pertaining to protocols for laser treatment. Any suggested protocols for treatment may be based upon the speakers' own clinical experience and should not be construed as Academy of Laser Dentistry recommended protocols.
Note: These presentations discuss investigational devices that may not yet have received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.

The Academy of Laser Dentistry (ALD) is a not-for-profit organization qualifying under Section 501c(3) of the U.S. Internal Revenue Code.The Academy of Laser Dentistry is an international professional membership association of dental practitioners and supporting organizations dedicated to improving the health and well-being of patients through the proper use of laser technology. The Academy is dedicated to the advancement of knowledge, research, and education and to the exchange of information relative to the art and science of the use of lasers in dentistry. Abstracts, presenter biographies, disclosure information, and product descriptions are published for educational purposes as submitted by the respective presenters and exhibitors. They do not necessarily represent the views of the Academy of Laser Dentistry. ALD is not responsible for the opinions expressed by the presenters, exhibitors, and advertisers. Written permission must be obtained by the Academy to audiotape, videotape, duplicate, and/or distribute any portion of the conference program or proceedings. The ALD Conference presents opportunities that may discuss investigational devices that have not yet received U.S. FDA approval or clearance for the specified clinical indications or describes off-label uses. Practitioners are advised to investigate and consider which medical devices and materials are cleared by the U.S. Food and Drug Administration for safety and efficacy and which are considered experimental, and which procedures are within the applicable scope of their license, competence, skills, and abilities, as established by their education, training, and experience. Clinicians are advised to review the specific indications for use of their devices and to review their operator manuals for guidance on operating parameters before attempting similar techniques on their patients.
© Copyright 2021 Academy of Laser Dentistry. All rights reserved.
|