ALD PEDIATRIC SYMPOSIUM - Wednesdays in January, February & March 2021 - 10 weekly sessions 17.5 CEUs
Pediatric Health - A Differential Diagnosis: Beyond Tethered Oral Tissues (TOTs)
A 10-Week Symposium Live and On-Demand
Download the Program Guide.
The ALD Pediatric Symposium will be held on our virtual platform. The best way to experience this event is live, but if you're not able to attend the live sessions due to time zones or scheduling conflicts, no problem! Your registration includes links to the recorded sessions which you'll be able to view after the event and earn up to 17.50 CEUs.
View the Schedule here.
Revising Tethered Oral Tissues (TOTs) is not just for breastfeeding. This 10-week CE virtual program takes dentistry to new levels of diagnosis 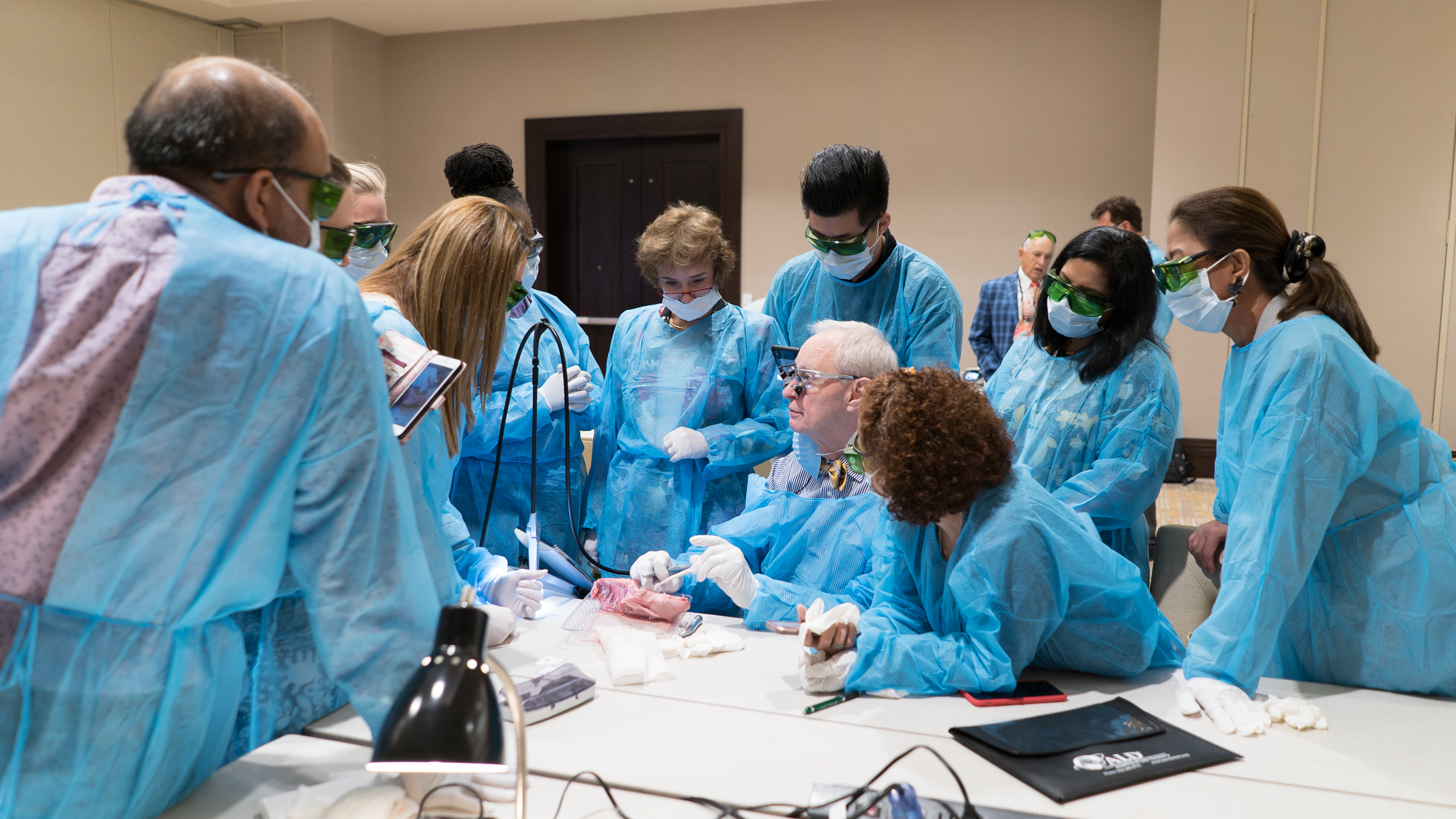 and treatment for systemic health from birth to old age. The program provides topics beyond tethered oral tissues. and treatment for systemic health from birth to old age. The program provides topics beyond tethered oral tissues.
Attendees will receive links to the recorded sessions after the Symposium ends.
Presentations include the following topics:
-
Brain development
-
Eliminating air induced reflux
-
Speech concerns
-
Preventing attention deficit disorder (ADD or ADHD)
-
Diagnosing obstructive sleep apnea (OSA) in children
-
Using lasers to stop snoring
-
Aftercare for surgery in children and adults
-
The role of myofunctional therapy
-
Examination of an infant for tots that includes more than just looking at an infant’s mouth
Educational Objectives:
- Understanding why revising the lingual frenum and other TOTs is not just for improving breastfeeding
- Understanding how untreated ankyloglossia may have long term effects on brain development, which may continue into adulthood
- How to do a proper assessment and exam to determine the existence of TOTs
- Learn who are the members of the assessment and treatment team for TOTs
Attendees can earn up to 17.50 CEUs for attending all of the sessions.
Registration fees: ALD Members $225 | Non-members $275.
Can't attend the live sessions? Register to receive links to the recorded sessions and earn up to 17.50 CEUs.
SPONSORS
SCHEDULE
|
|
|
|
|
Wednesday, January 6, 2021 | 7:30 pm ET
Larry Kotlow, DDS, Albany, NY, USA
Revising Restrictive Tethered Oral Tissues (RTOTs) Is Not Just for Breastfeeding
|
Wednesday, February 3, 2021 | 7:30 PM ET
Michael Gelb, DDS,MS, New York, NY, USA
Tongue as It Relates to Airway
|
Wednesday, March 3, 2021 | 7:30 PM ET
Benjamin Curtis, DDS, Canton, TX, USA
TOTs: Organizing for the Unexpected
|
|
Wednesday, January 13, 2021 | 7:30 PM ET
Kevin Boyd, DDS, Chicago, IL, USA
The Tongue and Its Relationship to Growth, Development, and Function of the Cranio-Facial-Respiratory Complex (CFRC)
|
Wednesday, February 10, 2021 | 7:30 PM ET
Sharon Vallone, DC, FICCP, South WIndsor, CT, USA
The Third Side of the Triangle: The Rationale for Pre- and Post-Surgical Chiropractic Care of the Infant with TOTs
|
Wednesday, March 10, 2021 | 7:30 PM ET
Edward R. Kusek, DDS, Sioux Falls, SD, USA; Vicki L. Neve, Sioux Falls, South Dakota, USA
Soft Tissue Procedures Other than Frenectomies and How Insurance Covers Them
|
|
Wednesday, January 20, 2021 | 7:30 PM ET
Michelle Emanuel, OTR/L, Cincinnati, OH, USA
Parent-Infant Bonding, Connection, CoRegulation and the need for earliest Myofunctional Therapy Intervention
|
Wednesday, February 17, 2021 | 7:30 PM ET
Vanessa Anderson-Smith, MA CCC-SLP COM, Sioux Falls, SD, USA
Setting Up Our Patients for Success: Why Pre- and Post-Frenectomy Therapy is Essential
|
|
|
Wednesday, January 27, 2021 | 7:30 PM ET
Barry Raphael, DMD, Clifton, NJ, USA
The Tongue and the Orthodontist: A Troubled Love Story
|
Wednesday, February 24, 2021 | 7:30 PM ET
David Thome, DDS, Mooresville, NC USA
Pediatric Airway and Applications of A Dual Wavelength Laser
8:15 PM ET
Anthony Bolamperti, DDS, Omaha, NE, USA
Non-surgical SnoringSolutions with a 9.3-micron Laser
|
|
SESSION DESCRIPTIONS
JANUARY
|
|---|
|

|
JANUARY 6, 2021 | 7:30 PM ET
- Larry Kotlow, DDS, Albany, NY, USA
Revising Restrictive Tethered Oral Tissues (RTOTs) Is Not Just for Breastfeeding
Restrictive tethered oral tissues (RTOTs) can have a profound impact on infant brain development, create air-induced reflux, speech concerns, and contribute to attention-deficit disorder (ADD) or attention-deficit hyperactivity disorder (ADHD) and obstructive sleep apnea (OSA) in children. The correct way to examine an infant for TOTs includes more than just looking at the infant’s mouth.
Educational Objectives
- Understand why revising the lingual frenum and other RTOTs is not just for improving breastfeeding.
- Learn how untreated ankyloglossia may have a long-term effect on brain development which may continue into adulthood.
- Discover how to do a proper assessment and exam to determine the existence of TOTs.
- Identify the members of the assessment and treatment team for RTOTs.
Disclosure: In the past Dr. Kotlow has provided laser educational presentations, videos and consultations for HOYA ConBio and Fotona’s PowerLase AT Spa and LightWalker Lasers. He has contributed to the development of infant safety goggles with Innovative Optics. At the present time, he receives honoraria for training and provides education for Convergent Dental. He is a beta tester of new upgrades and software for the Solea all-tissue carbon dioxide dental laser (9300 nm), as well as a dental consultant to and investor in Convergent Dental.
|
|

|
JANUARY 13, 2021 | 7:30 PM ET
- Kevin Boyd, DDS, Chicago, IL, USA
The Tongue and Its Relationship to Growth, Development and Function of the Cranio-Facial-Respiratory Complex (CFRC)
Ankyloglossia, also referred to as tongue-tie or short lingual frenum, along with restrictive upper- and/or lower-lip ties and frenula that tightly bind posterior perioral mucosa to buccal gingivae, are collectively classified as Tethered Oral Tissues (TOTs). Dr. Larry Kotlow has recently suggested that TOTs are only diagnosable as a pathologic condition when tight constriction contributes to impaired function of the tongue, lips, and perioral musculature. Researchers have identified restrictive ankyloglossia (RA) as often being a component of orofacial myofunctional disorders implicated in etiologies of the following malocclusion phenotypes: transverse skeletal deficiency, anterior open-bite, high-angle mandibular growth, and high narrow palate. Other investigators have shown an association between restricted tongue mobility, narrowing of the maxillary dental width, elongation of the soft palate, and a high-arched palate, and, if left untreated at birth, RA is associated with obstructive sleep apnea syndrome (OSAS) at later age. Given that certain malocclusion phenotypes often associated with RA, specifically, transverse deficiency of the maxilla and/or mandible, sagittal deficiency of the mandible and/or maxilla, vertical skeletal maxillary excess or deficiency and high narrow palatal vault, it seems a medically indefensible position to not identify potentially problematic RA with validated screening tools, such as those published by Kotlow and Hazelbaker, as early in a child’s life as might be feasible to do so (i.e., under the age of six); and furthermore, when identified and diagnosed by a qualified health professional, it also seems indefensible to not offer appropriate intervention, or referral for intervention, by a qualified professional, for not only RA revision, but also for the correction of the RA-associated malocclusion traits that might present as a co-morbidities.
Educational Objectives
- Explain why restrictive ankyloglossia (RA) should be understood as a possible etiological factor contributing to orofacial myofunctional disorder (OMD), non-syndromic early (under age 6) childhood malocclusion (ECM), and pediatric sleep-related breathing disorder/obstructive sleep apnea (SRBD/OSA).
- Review how RA may be assessed for severity through utilization of validated screening assessment tools as early in a child’s post-natal life as might be feasible to do so.
- Appreciate why RA should be treated by a qualified and experienced medical or dental professional as a possible effective adjunct to other interventions aimed at correcting craniofacial-respiratory complex disease co-morbidities.
Disclosure: Dr. Boyd has no financial interests in any companies.
|
 |
JANUARY 20, 2021 | 7:30 PM ET
- Michelle Emanuel, OTR/L, Cincinnati, OH, USA
Parent-Infant Bonding, Connection, Co-Regulation and the Need for Earliest Myofunctional Therapy Intervention
How do babies and parents bond, connect, and co-regulate? What do these words actually mean and how do these processes translate for babies and families who are struggling to find the balance of feeding, oral dysfunction, and tethered oral tissues? One thing is certain, oral dysfunction causes stress and can interrupt the primal and innate capabilities of loving parents. Michelle will discuss how to bridge these gaps and promote connection, as well as ease, through professional interactions, procedures, and recommendations. Additionally, she will discuss the earliest application of myofunctional science for pre-crawling babies, the physiologic rationale, and how this promotes optimal craniofacial respiratory development.
Educational Objectives
- Identify two key aspects of parent / infant bonding and attachment.
- Understand the meaning of co-regulation and how that affects the release of tethered oral tissues.
- Describe two ways myofunctional therapy is essential for babies.
Disclosure: Michelle receives compensation from TummyTime! Method.
|
 |
JANUARY 27, 2021 | 7:30 PM ET
-
Barry Raphael, DMD, Clifton, NJ, USA
The Tongue and the Orthodontist: A Troubled Love Story
Orthodontists have known about the role of the tongue in facial growth and malocclusion for over a century, but have often forgotten this knowledge. Orthodontic specialist Dr. Barry Raphael will tell the story of his own troubled relationship with The Tongue and how he turned it into a collaborative partnership at best, and indeed, a stormy love affair at worst. He will look at how his orthodontic training did not prepare him for the changes that are occurring in orthodontics today and how a new way of thinking about the tongue, its function, and its behavior have now become a standard part of his integrative orthodontic practice.
Educational Objectives
- Summarize the role of the tongue in facial growth and development.
- Review the role of the tongue in airway function.
- Specify the three components of assessing and treating airway flow limitation.
- Appreciate the integrative model of orthodontics as a model for the future of all of dentistry.
Disclosure: Dr. Raphael is the owner of the Raphael Center for Integrative Orthdontics and founder of the Raphael Center for Integrative Education.
|
| FEBRUARY |
|---|
|

|
FEBRUARY 3, 2021 | 7:30 PM ET
- Michael Gelb, DDS,MS, New York, NY, USA
Tongue as It Relates to Airway
Tongue-tie, low tongue posture, and low tone are often associated with breathing-related sleep disorders (BRSD). All of these tongue qualities are associated with a narrow palate, nasal disuse, and mouth breathing perpetuating a downward spiral and altering facial growth. Optimizing tongue movement, posture, and tone following myofunctional therapy is often the first step in improving airway function and volume. This presentation will explore identification of children with craniofacial risk factors for BRSD with suggested solutions. AirwayCentric pediatric dentistry is dedicated to improved development of the prefrontal cortex and neurobehavioral and neurocognitive function. The role of the tongue in AirwayCentric pediatrics will be explored.
Educational Objectives
- Identify craniofacial risk factors in BRSD.
- Become familiar with the Pediatric Sleep Questionnaire or Sleep Inventory.
- Understand the role of the pediatric dentist in the Airway team.
- Describe the association between BRSD and attention-deficit disorder (ADD).
Disclosure: Dr .Gelb has a consulting agreement with ProSomnus.
|
|

|
FEBRUARY 10, 2021 | 7:30 PM ET
- Sharon Vallone, DC, FICCP, South WIndsor, CT, USA
The Third Side of the Triangle: The Rationale for Pre- and Post-Surgical Chiropractic Care of the Infant with TOTS
Chiropractors and other manual therapists can play a key role in the care of infants with feeding difficulties related to TOTs. The role of the chiropractor is to evaluate and diagnose functional aberrations as they relate to infant biomechanical and neurologic integrity. Presurgical evaluation and treatment of such conditions have the potential for preventing unnecessary surgery (revealing that, in fact, the TOTs were not the source of the dysfunctional oral motor development) or will support the surgical intervention by reducing any compensatory biomechanical or soft tissue restrictions that could interfere with the ability of the dentist/surgeon to access a clear field for surgery. Compensatory soft tissue adhesions, muscular asymmetry, or articular misalignment can result in decreased mandibular gape, taut peri-oral, submandibular, and masticatory musculature. Poor cervical range of motion restricts the infant’s ability to extend at the cranial base and widely gape, and plays a role in retraction of the mandible. As an anchor for the lingual musculature, the hyoid bone is an integral part of the evaluation and treatment of breastfeeding dysfunction, and its potential role in airway obstruction will also be examined. Post-surgical care has a supportive role in helping to resolve compensatory musculoskeletal issues and in the neurologic integration of the structural changes as a result of releasing the oral tissues.
Educational Objectives
- Summarize what chiropractic care entails for the infant and how it fits into the collaborative care of the infant with dysfunctional feeding issues.
- Understand the difference between neuromusculoskeletal dysfunction and TOTs as they relate to oral motor function of the infant with dysfunctional feeding issues.
- Describe what pre- and post-chiropractic care comprises for the infant who has dysfunctional feeding issues.
Disclosure: Dr. Vallone has reported no conflicts of interest.
|
 |
FEBRUARY 17, 2021 | 7:30 PM
- Vanessa Anderson-Smith, MA CCC-SLP COM, Sioux Falls, SD, USA
Setting Up Our Patients for Success: Why Pre- and Post-Frenectomy Therapy is Essential
Time and time again it has been found that a frenectomy can make significant and positive impacts in a child’s eating, speaking, and airway functions. However, what happens before and after the release is vital in setting our patients up for achieving ideal function and receiving overall benefit from the procedure. This presentation will discuss why pre-frenectomy therapy is essential in not only properly preparing the oral structure but also encouraging the cooperation of the patient pre- and post-procedure. Also included is a discussion of how and why therapy after frenectomy aids in teaching patients optimal movement and function following a structural change.
Educational Objectives
- Describe how the therapy process is important to a frenum release.
- Summarize what a functional oral assessment entails.
- Explain how pre-frenectomy therapy can increase cooperation and tolerance of the patient during the procedure and aftercare.
Disclosure: Vanessa is a TalkTools instructor and is paid to create and teach courses using the TalkTools techniques. She is also an independent contractor for Little Sprout Speech, specifically a moderator on social media platforms for the Feed The Peds: The Myo Membership program.
|
 |
FEBRUARY 24, 2021
7:30 PM
- David Thome, DDS, Private Practice, Mooresville, NC USA
Pediatric Airway and Applications of a Dual-Wavelength Laser
A better airway means better babies and better children/adults. This presentation is a high-level overview of current treatments offered in pediatric dentistry and how lasers can be incorporated for airway enhancement. Topics include: NightLase® – pediatric applications and the minimally invasive approach to better breathing with dual laser therapy; Tongue ties – how these conditions contribute to decreased oxygenation of cells; Mouth breathing – less oxygen, more cavities, prevents reset of immune system and endocrine system; Frenectomies – improve function of tongue for feeding and breathing; Appliances – HealthyStart® habit-correcting appliances help keep the mouth closed and airway open.
Educational Objectives:
- Discuss the pediatric airway and use of laser therapy with a dual laser system.
- Learn how to screen for breathing and speech disorders.
- Specify appliances for breathing disorders and habit correction.
Disclosure - Dr. Thome lectures for Fotona and receives a modest honorarium for these activities.
|
|

|
8:15 PM
- Anthony Bolamperti, DDS, Omaha, NE, USA
Non-surgical Snoring Solutions with a 9.3-micron Laser
Did you know that 67% of the population snores? People who snore typically have an airway issue, and that can complicate other systemic health issues. One major airway issue is tethered oral tissue (TOT), which may cause airway obstruction. TOTs needs to be identified and treated at the earliest age possible. When it goes undiagnosed and treated, it can lead to major health complications and negatively affect overall function. In the past, patients who needed intervention for snoring could opt for uncomfortable oral appliances, uncomfortable pull-forward splints, or invasive orthognathic surgery. With Solea® Sleep, these patients now have a fast and effective alternative. This is an easy-to-administer protocol for use with a 9.3-micron all-tissue dental laser (Solea, Convergent Dental, Needham, Mass., USA) that provides patients with rapid relief by tightening the soft palate and reducing vibrations that cause patients to snore. Unlike surgical procedures that require long and painful recoveries, Solea Sleep is a non-surgical treatment that allows patients to immediately return to their daily routines with little to no discomfort.
Educational Objectives
- Summarize available treatment solutions for tethered oral tissues.
- Discuss the diagnosis of snoring.
- Describe treatment of snoring with the Solea Sleep protocol.
Disclosure: Dr. Bolamperti lectures for Convergent Dental and receives a modest honorarium for these events.
|
| MARCH |
|---|
|

|
MARCH 3, 2021 | 7:30 PM
- Benjamin Curtis, DDS, Canton, TS, USA
TOTs: Organizing for the Unexpected
We always anticipate that our TOTs procedures will go as planned, but that is not always the case. This discussion examines issues that can arise in TOTs care and focuses on helping to organize for these unexpected events. One almost unavoidable side effect of TOTs procedures is bleeding. This discussion will identify pre- and post-operative factors that place patients at higher risk for bleeding and review ways to help manage uncontrolled bleeding if it should occur during or after the procedure. This discussion will also look at patient selection for TOTs procedures with a comprehensive approach based on patient need, health history, and behavior. From this, we can best plan the proper management of care for the patient. This will help us identify when to monitor the TOTs, proceed with TOTs treatment, or refer out. Good patient selection is always an important factor in avoiding unexpected outcomes. Many procedural difficulties can be avoided by beginning with a solid pre-op and post-op care plan that is well communicated to the family. While a good game plan is crucial, it is also important to remain adaptive in your protocol. This discussion will identify ways to be flexible and troubleshoot your pre-op and post-op care plan to best fit the specific needs of patients and their families. First-time mothers, high-maintenance moms, and difficult patients are not uncommon in TOTs practices, but identifying them early and adapting your pre-op and post-op care plan can help to improve their experience and the results of the procedure. We will conclude with a discussion on low socio-economic status (SES) patients where payer source may be a hindrance to proper or ideal treatment and care. This population tends to be a patient group where access to care is a big problem and our classic team approach to TOTs procedures may not be realistic due to limited finances, poor insurance benefits, and many other confounding factors. This population challenges us to think outside the box, and in this discussion, we will look at ways to be adaptive in managing their TOTs care. Unexpected things happen, but it is rising to the occasion for your patient in that moment that can make all the difference. It is my hope that we shall rise, and rise together we shall.
Educational Objectives
- Identify risk factors for bleeding during TOTs care and be prepared to manage uncontrolled bleeding if it should arise.
- Comprehensively select patients based on need, health history, and behavior, and identify when to monitor, proceed, or refer.
- Begin with a solid pre-op and post-op care plan while remaining flexible and adaptive to the specific needs of the patient and family.
- Think outside the box for low SES patients and keep an adaptive team approach to TOTs care.
|
|
|
MARCH 10, 2021 | 7:30 PM
- Edward R. Kusek, DDS, Sioux Falls, SD, USA
- Vicki L. Neve, Sioux Falls, South Dakota, USA
Soft Tissue Procedures Other than Frenectomies and How Insurance Covers Them
This presentation will show how you can use your laser to increase your return on investment by performing soft tissue procedures such as biopsies, aesthetic crown lengthening, ovate pontics, distal wedges, and periodontal treatments. The presenters will share how to maximize benefits for your patient with dental and medical insurance.
Educational Objectives
- Increase return on investment with your dental laser by doing procedures other than frenectomies.
- Define steps to complete laser-assisted biopsies.
- Learn how to use your dental laser to reduce the need for referral.
- Specify proper dental and medical codes to submit for your patient’s maximum benefits.
Disclosure: Dr. Kusek lectures for Ultradent Products and receives an honorarium. He consults with laser companies Biolase, Great Plains Technologies, Ultradent, and Convergent Dental, and with Straumann on dental implants.
Disclosure: Vicki has reported no commercial affiliations or personal conflicts of interest.
|
SPONSORS
ALD Organization Disclosure - Disclaimer on Protocols and Opinions
The views expressed and the opinions and materials presented during a presentation represent the personal views and opinions of the individual speakers and do not necessarily represent the views and opinions of the Academy of Laser Dentistry. The Academy of Laser Dentistry assumes no responsibility for the content of the presentations made by individual speakers pertaining to protocols for laser treatment. Any suggested protocols for treatment may be based upon the speaker's own clinical experience and should not be construed as Academy of Laser Dentistry recommended protocols.
Note: These presentations discuss investigational devices that may not yet have received U.S. FDA approval or clearance for the specified clinical indications, or describes off-label uses.

These programs are intended to provide 1 ADA CERP credit of continuing education for dentists or other dental professionals.
|













 and treatment for systemic health from birth to old age. The program provides topics beyond tethered oral tissues.
and treatment for systemic health from birth to old age. The program provides topics beyond tethered oral tissues.